EMINENT-ICH Trial
Welcome to the EMINENT-ICH website!
The EMINENT-ICH trial is a national multi-center trial in Switzerland investigating the role of early minimally invasive endoscopic hematoma removal in spontaneous supratentorial intracerebral haemorrhage.
On this website you can find more information regarding the trial by using the sidebars to help you navigate the site.
Kind regards on behalf of the EMINENT-ICH study team
PD Dr. med. Jehuda Soleman
Information for patients
General study information
Why do we do this study?
Spontaneous brain bleedings, also called spontaneous intracerebral hematomas (SIH), are the2nd most common form of stroke and affect around 2500 patients annually in Switzerland. After a year, approximately half of these patients die while those who survive are to mostly severely disabled.
To date, the gold standard remains medical treatment (BMT), consisting of blood pressure control and intensive care treatment.
Surgical care consists of hematoma removal through open brain surgery which showed minimal effect on survival, at the cost of a higher percentage of patients with disabilities and is thus not considered superior to BMT.
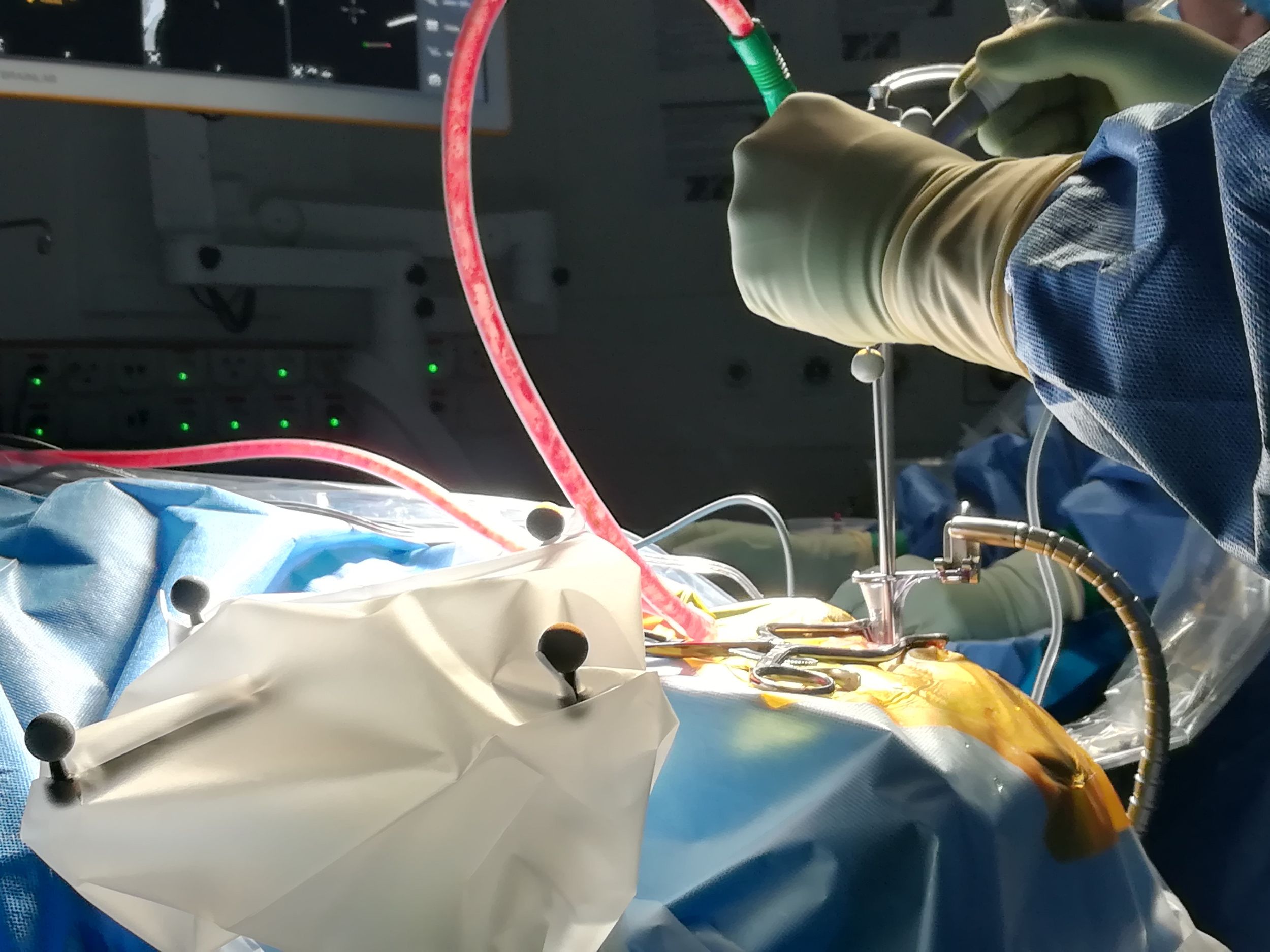
Minimally invasive endoscopic surgery is a procedure, where the approach to the brain is minimally invasive since the operative field can be seen through a camera. In low quality studies this technique has shown improved rates of survival and less disabled patients compared to BMT and open brain surgery. In addition, the operative side-effects compared to open brain surgery are reduced by the endoscopic technique. However, to date, no large high-quality study has confirmed that minimally invasive endoscopic surgery is superior to BMT.
Further, to date, most studies looking at the benefit of surgery in case of SIH, either operate ultra-early (within 6 hours) or within 48-72 hours from the bleeding event. When analyzing the scientific literature, it seems that ultra-early surgery is risky, since it leads to more bleeding complications, while removal after 48-72 hours might be too late, since the blood degradation products within the brain may further damage the vital brain tissues surrounding the hematoma. Therefore, hematoma removal within 6-24 hours after a bleeding event seems an ideal time point for a minimally invasive endoscopic hematoma removal.
What does the study want to achieve?
With the EMINENT-ICH trial, we intend to assess in a randomized controlled, multi-center fashion the potential superiority of early endoscopic hematoma removal over BMT in patients with SIH, that means we want to see, whether or not endoscopic surgery leads to a better outcome and improved mortality rates for patients with SIH.
What happens in the study?
Patients will undergo a screening based on predefined eligibility criteria and if eligible, they will be randomly assigned to either minimally invasive endoscopic surgery and BMT or BMT alone. We intend to include patients across Switzerland with SIH of a predefined hematoma size suffering significant disabilities due to the bleeding and who are not older than 85 years of age. The surgical group will be treated within 6 to 24 hours after bleeding onset. Patients of both groups will be clinically assessed during hospital stay and after rehabilitation. The degree of disability at 6 months, which represents the primary outcome of the study, will be assessed in our out-patient clinic. Additionally, we assess patient reported outcome measures (PROMs) like patient satisfaction and quality of life. The study participants will experience 6 visits over a duration of 6 months in total.
In the following table you see what the different visits will include. All of this is routine clinical practice and will not affect your treatment.
What makes EMINENT-ICH special?
During the planning of this study, we worked closely together with affected patients, relatives/caregivers of affected patients and representatives of the patient organization EUPATI Switzerland to make this study patient friendly and cover the needs of affected patients and their caregivers.
As a result, we identified quality of life and cognitive outcome as needs of patients, which are, to date, underreported in the field of SIH treatment. We improved our visit schedule, and we collaboratively designed an easy to understand informed consent form and lay summary. We also have planned to include a patient expert in our study supervision team (Data and Safety Monitoring Board) who will assess the risk and benefit ratio of this study for patients throughout its conduct.
After the results of the study are available, we will work with patient organization representatives to make sure that the results are made accessible to the affected patients who can hopefully make use of them.
Lastly, together with our representatives, we will assess the impact of patient and public involvement on our study to gain insights on how to improve the collaboration between the patients and public and the researchers for future research.
Who can participate
All patients meeting the eligibility criteria can be included in this trial if they want to participate. We herein list only the most important eligibility criteria.
Inclusion criteria:
- Patient age ≥ 18 and <85
- Spontaneous brain bleeding with a volume of at least 20 mL
- A neurological impairment i.e. hemiparesis or decreased consciousness
- Surgery can be performed within 24 hours after bleeding onset
- Informed consent present
Exclusion criteria:
- Brain bleeding due to tumor, vascular malformation or trauma
- Bleeding in the cerebellum
- Impaired coagulation
- Prior disability
- Pregnancy
Risks and benefits
Most of the risk in this study come from the underlying disease of intracerebral haemorrhage. However, as with every surgical procedure there exist some very rare risk like rebleeding and wound infections. Your treating physician will inform you about the specific risk if you have any further questions.
As we are looking for a potential improvement trough surgery, there can but not necessarily has to be an improvement of disability in the daily life. If randomized to the best medical treatment arm you will receive the current best care for intracerebral haemorrhage.
Video
Further information
Further information can be found at the Swiss national clinical trial portal KOFAM (german) and under the ClinicalTrials registry (english).
Contact
If you have any further inquiries regarding the EMINENT study, please contact:
Dr. Tim Hallenberger
Sub-Investigator
Department of Neurosurgery
University Hospital Basel
Spitalstrasse 21, CH-4031 Basel
Information for collaborators
Background, Design, Objectives and Outcomes
Background
Spontaneous supratentorial intracerebral haemorrhage (SSICH) is the second most common form of stroke and accounts for approximately 2500 cases in Switzerland annually. The prognosis is very poor with nearly half of the patients dying within one year after haemorrhage.
Treatment options for SSICH remain ambiguous and consist of either the current gold standard, best medical treatment, or surgical hematoma evacuation. Neither the best medical treatment nor the established surgical mainstay (conventional craniotomy) have shown relevant improvement of survival or functional outcome rates. We therefore propose a minimally invasive approach with early image-guided endoscopic surgery performed within 24 hours. Endoscopic surgery was shown to be safe and effective, however large trials analyzing the benefits of endoscopic surgery are lacking. We therefore propose that an earlier, more complete and more rapid hematoma evacuation will improve the functional outcome and mortality rates in these patients.
Design
This is a single-center, two-arm, open-labelled randomized controlled trial in superiority fashion.
Objectives and outcomes
Primary objective:
The primary objective is to show superiority of early minimally invasive image-guided hematoma evacuation additionally to BMT compared to BMT alone in functional outcome rates at 6 months in patients with SSICH.
Secondary objectives are:
- to show superior survival rates of patients in the ES arm
- to study patient reported quality of life after treatment for SSICH at different time points (3 and 6 months after intervention)
- to study patient satisfaction with the outcome after treatment for SSICH at different time points (7 days, 3 months and 6 months after intervention)
- to study cognitive outcome in patients after treatment for SSICH at different time points (7 days, 3 months and 6 months after intervention)
- to study the morbidity rates of patients in both treatment arms
- to study the efficacy of ES in reducing the hematoma volume
- to study the change in focal neurological deficits exhibited by the patients after treatment.
- to study the temporal evolution of serum biomarkers (Neurofilament light-chain subunit (NfL), Glial Fibrillary Acidic Protein (GFAP), S100 calcium-binding protein B (S100B), IL-1α and β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12p70 and TNF-α) and their change in relation to early hematoma ES.
Primary outcome:
- Good functional outcome 6 months after treatment, measured by the mRS. Good functional outcome is defined as a mRS of ≤3 points and will be assessed as binary outcome at 6 months after treatment.
Secondary outcomes:
- The mortality rate as measured by death of a participant at 6 months after intervention.
- Patient reported outcome measures at 7 days (Patient satisfaction and cognition), 3 and 6 months after intervention, those being:
- Patient and caregiver quality of life as assessed by the PROMIS® questionnaire
- Patient Satisfaction as assessed by a short survey on a scale of 1-5
- Patient cognitive outcome as assessed by the MOCA® Test
- The morbidity rate, meaning occurrence of:
-
- Ischemic stroke
- Recurrent SSICH (defined as any radiologically confirmed increase in hematoma volume postoperative/follow-up that is either asymptomatic or associated with a worsening of the focal-neurological deficit by ≥4 points on the NIHSS and/or a decrease in consciousness by ≥2 points on the GCS)
- Epileptic seizure
- Surgical site infection (intervention group only)
- Any need for open neurosurgical procedures
- Infections (i.e. pneumonia, urinary tract infection)
- Any other not defined complication that prolongs the hospital stay and/or leads to further treatment not envisaged in the original treatment plan.
- The occurrence of any of these events 6 months after intervention:
-
- The change of focal neurological deficit measured by the NIHSS, from baseline to 6 months after intervention as a continuous variable
- The time to intervention, defined as the period from symptom onset/last seen well to start of surgery (start surgical measures, i.e. positioning of patient) or start of medical treatment (admission of first treatment of BMT)
- The temporal evolution of serum levels of the prespecified biomarkers as continuous variable from start to 6 months after intervention
- The total time spent on the intensive care unit (ICU)/stroke unit as a continuous variable from the first admission to the ICU/stroke unit to discharge from ICU/stroke unit at 7 days/discharge after intervention
- The total time spent in intubation measured in minutes from the start of intubation to extubation as specified in the anesthesiology report at 7 days/discharge after intervention
- Outcomes/Measurements applying to the intervention group only:
-
- The proportion of hematoma volume reduction rate (goal ≤15% of its initial volume). The hematoma volume reduction rate will be a binary variable
- The relative (percentage) reduction or increase of hematoma volume from baseline admission cCT to postoperative cCT directly after surgery as a continuous variable (final value)
Eligibility
Patients
Herein you will find the eligibility criteria for the EMINENT-ICH trial.
Inclusion criteria:
- Patient age ≥ 18 and <85
- Spontaneous supratentorial intracerebral hemorrhage (SSICH), defined as the sudden occurrence of bleeding into the lobar parenchyma and/or into the basal ganglia and/or thalamus that may extend into the ventricles confirmed by imaging
- SSICH volume ≥20 mL <100 mL (measured using the formula A * B *C2)
- Stable clot volume defined as absence of increase of >33% (as assessed using the formula (A * B * C)/2) of initial clot volume on follow-up imaging.
- A focal neurological deficit consisting of either
- clinically relevant hemiparesis (≥4 motor points on the NIHSS for facial palsy, motoric upper and lower extremities combined)
- clinically relevant motor or sensory aphasia (≥2 points on the NIHSS)
- clinically relevant hemi-inattention (formerly neglect, 2 points on the NIHSS)
- decreased level of consciousness (GCS≤13)
- Presenting GCS 5 - 15 (in intubated patients GCS assessment will be performed after Rutledge et al. (Figure 2) or if impossible, the last pre-intubation GCS will be used)
- Endoscopic hematoma evacuation can be initiated within 24 hours after the patient was last seen well/symptom onset
- Informed consent of patient (only for patients able to consent)
Exclusion criteria:
- SSICH due to known or suspected structural abnormality in the brain (e.g. vascular malformation, aneurysm, AVM, brain tumor) and/or brain trauma and/or hemorrhagic conversion of an ischemic infarction
- Multiple simultaneous intracranial hemorrhages (e.g. multifocal ICH, cSDH, aSDH, SAH)
- Infratentorial hemorrhage or midbrain extension/involvement of the hemorrhage
- Coagulation disorder (including anticoagulation) with an INR of >1.5 which cannot be pharmacologically reverted until the planned time of evacuation
- Positive history of current pregnancy, breast-feeding, or positive pregnancy test [either serum or urine] in premenopausal women
- Relevant disability prior to SSICH (mRS >2)
- Any comorbid disease or condition expected to compromise survival or ability to complete follow-up assessments through 180 days (e.g. bilateral fixed dilated pupils)
Study centers
If you are interested to participate as a collaborator, please check the following eligibility criteria for your center:
- Must have a stroke unit or be certified as stroke center
- Must have neurosurgical OR with endoscope and some form of neuronavigation
- Must be able to conduct directly postoperative CT for assessment of hematoma evacuation rate
- Must have 24-hour neurosurgical and neurological service
Trial progress and active recruiting sites
Visit schedule
Following you will find the visit schedule for the EMINENT-ICH trial.
Video
Trial documents
Contact and dates of training
Contact
PD Dr. Jehuda Soleman
Principal Investigator
Department of Neurosurgery
University Hospital Basel
Tim Hallenberger
Sub-Invesitgator
Department of Neurosurgery
University Hospital Basel
Birsel Klein-Reesink
Study coordinator
Department of Neurosurgery
University Hospital Basel
Training dates
