Our expertise in bladder cancer
Bladder cancer is the tenth most common cancer in Europe, affecting men three times more often than women. We are experts in the field and the only center for bladder cancer in the Basel region.
At the University Hospital Basel, specialists from urology, radiation oncology, oncology and various other disciplines work closely together. Patients thus have access to modern forms of therapy, highly qualified diagnostics and optimal treatment for bladder cancer.
Facts and figures
>1000
Patients assessed and treated at the Urological Tumor Center on an interdisciplinary basis / year
>360
Patient cases with tumors in the renal pelvis, ureter and bladder discussed at the tumor board / year
30-40
robot-assisted urinary bladder removals / year
>500
Remedy applications in the urinary bladder / year
Find out more about our expertise
Support from a multidisciplinary team
- Interdisciplinary consultation hours with specialists in urology, radiation oncology and oncology.
- Extensive experience in bladder tumor therapy.
- Comprehensive personal consultation and, where possible, customized therapy recommendations.
- Specialized tumour aftercare.
Comprehensive diagnostics and research
- The most modern image diagnostics available.
- Identification of cancer genes and proteins that control uncontrolled tumor growth and are potential therapeutic targets.
- Continuous further development of diagnostics and therapy in the laboratory.
- Innovative therapies through our active participation in national and international clinical research studies.
State-of-the-art surgery
- Leading university center for oncological-robotic therapy of the urinary tract.
- Endoscopic removal of urinary bladder tumors (TUR-B) and removal of the urinary bladder (cystectomy) with optimized urinary diversion and bladder-preserving therapies.
- Specialized center for radical removal of the entire bladder using the DaVinci system.
Our team


PD Dr. Jan Ebbing
Leitender Arzt
Urologie
Teamleiter Robotische Chirurgie der Harnblase


Our specialists provide insights into their areas of expertise
Imaging: MRI of the urinary bladder
Multi-parametric magnetic resonance imaging (MRI) of the bladder provides us with detailed information about the location and extent of bladder tumors.
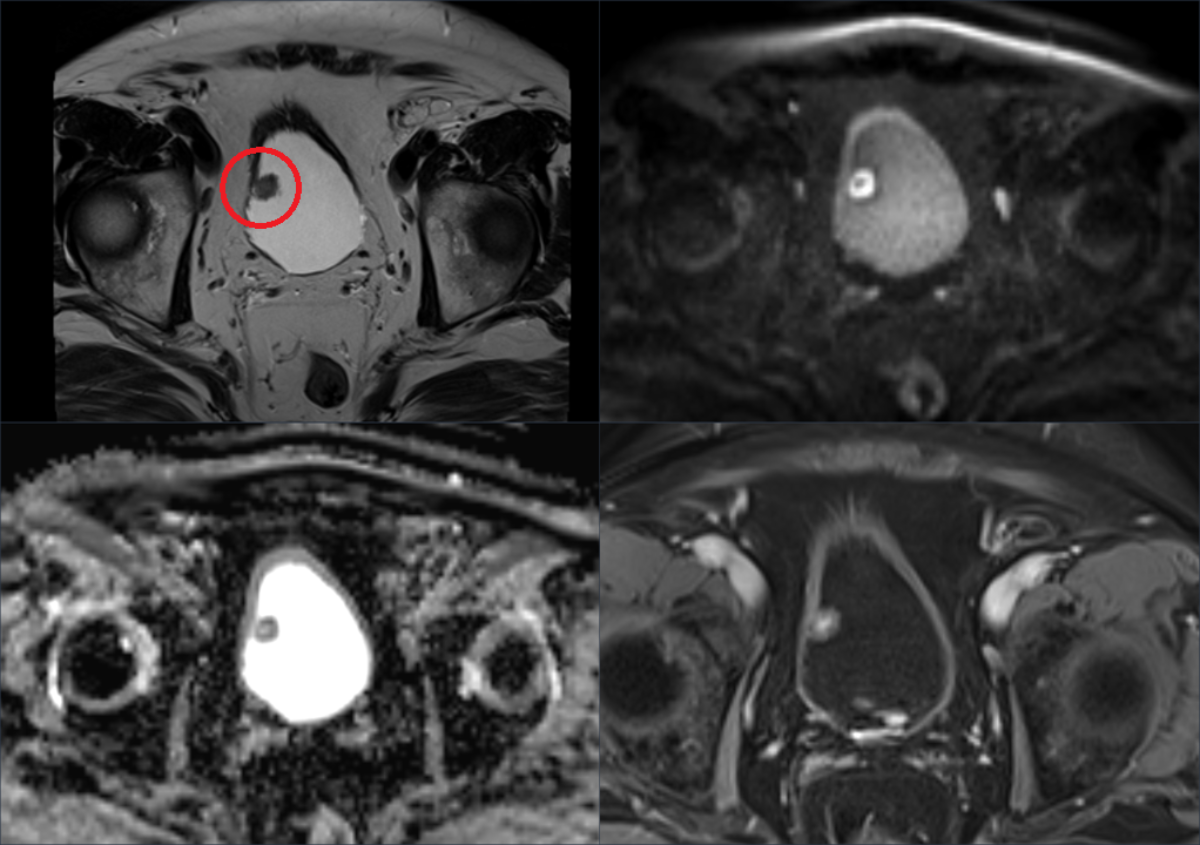
Example of a multiparametric MRI of the urinary bladder. Four different sequences (parameters) show the local extent of a bladder carcinoma on the right bladder roof (red circle, top left).
An MRI helps us with this
An MRI of the bladder allows us to assess the size of the tumor, the depth of infiltration into the bladder wall and surrounding tissue, and the presence of lymph node metastases. This imaging supports doctors in staging and selecting suitable treatment options.
In addition, MRI can be used in long-term follow-up after treatment has been completed for the early detection of relapses or metastases.
Prof. D. Boll, Deputy Head of Radiology and Nuclear Medicine
Application of remedies in the urinary bladder
If you need bladder irrigation for bladder cancer, our experienced and trained team will be happy to help you. Thanks to our expertise in this form of therapy and the wide range of treatment options, we treat patients from all over Switzerland and nearby countries at our center.
You will receive a medically approved treatment plan in accordance with the guidelines of the European Society of Urology. Your individual appointment requests will of course be taken into account as far as possible.
Your bladder irrigations are administered via a urethral catheter in a specially created treatment lane. We make sure that the therapy is as painless and side-effect-free as possible.
Our specially trained staff are on hand to support you during and after your treatment.
Prof. C. Rentsch, Head Physician Urology
H. Püschel, Head Study Nurse Urology
What our patients say
" ... today (hopefully) marks the end of a program that you can easily do without. But if such treatment is necessary, a patient can be grateful to meet competent and friendly people. From the very first day, you managed this with aplomb and allayed my fears.
In this respect, what a miracle, we live in a progressive time, which thanks to medicine extends life enormously. For this reason, as well as for the entire treatment, I would like to say a big thank you! "
Lothar Thomma, September 2023
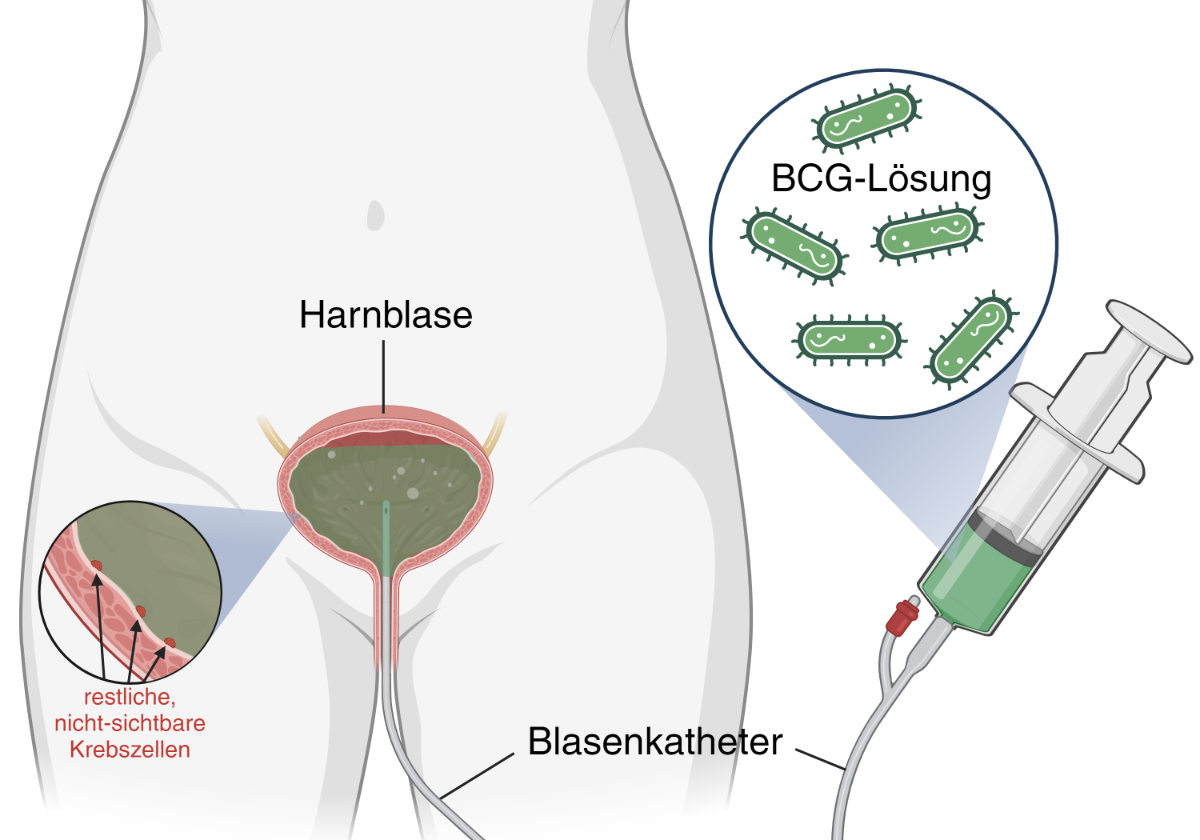
Immunotherapy with BCG instillations.
Illustration created with BioRender.com.
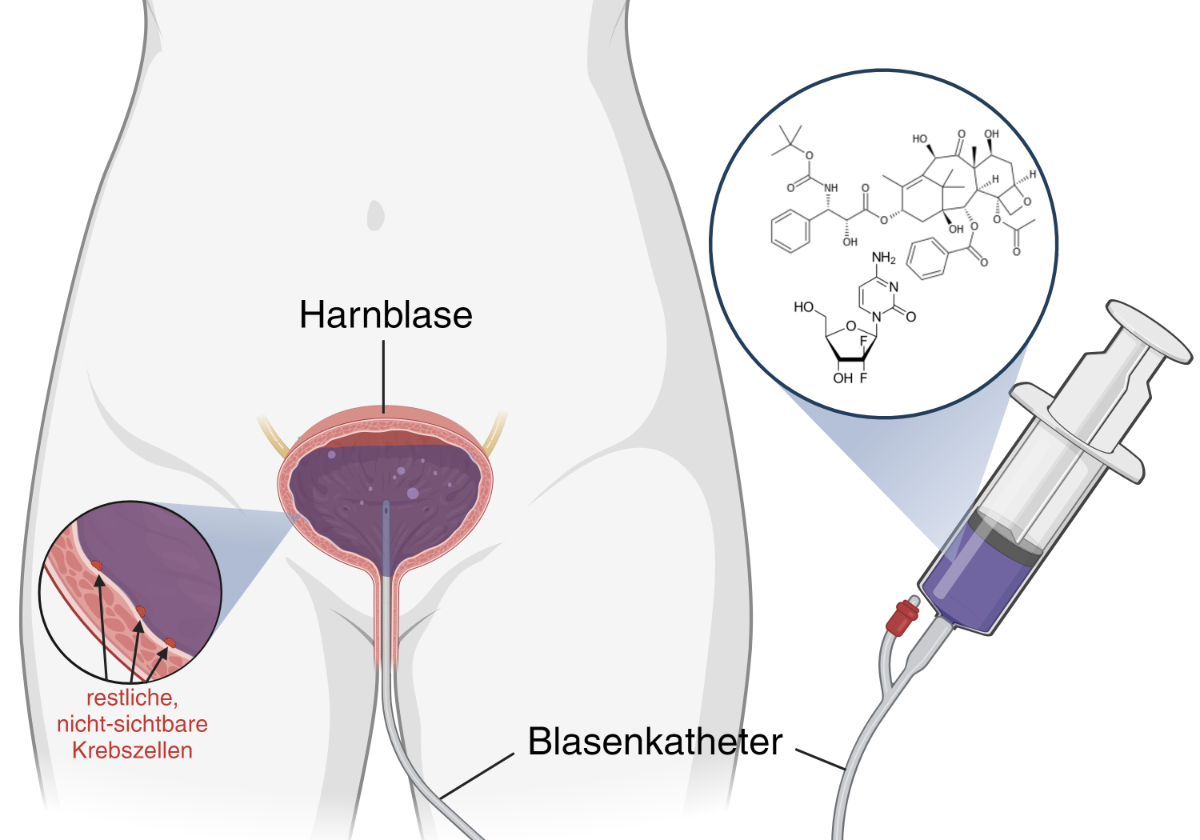
Intravesical chemotherapy instillations.
Illustration created with BioRender.com.
Robot-assisted urinary bladder removal
The Urology Clinic at the University Hospital Basel is one of the few clinics in Switzerland that performs minimally invasive and robot-assisted bladder removal for advanced (muscle-invasive) bladder cancer.
The DaVinci® Xi system from Intuitive Surgical™, which is currently the most modern system on the market, is also used at the USB.
©2023 Intuitive Surgical Operations, Inc.
Advantages of robotic surgery
Robotic cystectomy (bladder removal) with intracorporeal urinary diversion is a state-of-the-art surgical approach that offers several advantages for patients with bladder cancer. This minimally invasive technique uses robotic technology to remove the bladder. Intracorporeal means that the urinary diversion (urinary stoma/conduit or neobladder) does not require a large open abdominal incision, but is also performed using robot-assisted keyhole surgery. The robot-assisted procedure is associated with the following scientifically proven advantages, among others.
- Faster recovery and shorter hospital stays compared to open surgery.
- Reduced post-operative pain and improved quality of life.
- Reduced risk of bleeding and less need for blood transfusions.
- More precise removal of malignant tissue and improved visualization during surgery.
- Comparable oncological results to conventional open surgery, which underlines the effectiveness of this procedure.
At the University Hospital Basel, in addition to the conventional urinary stoma (ileum conduit), the much more complex form of urinary diversion using an orthotopic ileum neobladder is performed completely intracorporeally (see definition above) with the DaVinci® Xi robot. This highly complex form of urinary diversion is only performed minimally invasively in very few centers with proven experience in robot-assisted surgery.
Our robotic surgeons have proven expertise in this field and have been trained at the renowned Karolinska University Hospital in Stockholm, Sweden, one of the world's best-known pioneer hospitals for robot-assisted cystectomy.
PD Dr. J. Ebbing, Head Physician Urology
Radiotherapy and chemotherapy as an alternative to radical removal of the bladder
In the case of a tumor that has already grown into the muscle layer of the bladder wall, a combination of radiotherapy and chemotherapy can be used as an alternative to radical removal of the bladder.
Adaptive radiotherapy of a bladder tumor. The red area shows the maximum radiation dose directed at the bladder. Green is the lower dose range, which is used to cover the lymph nodes around the bladder in order to combat any existing tumor cell nests.
The latest technology in adaptive radiotherapy
This procedure is suitable for patients whose tumors are smaller than 6 cm, have no precancerous lesions distributed on the bladder mucosa and still have good urinary flow control. The chances of success are similar to a radical removal of the bladder.
Before treatment, a cystoscopy is performed again so that as much of the tumor as possible can be removed. Subsequently, the entire bladder is irradiated every working day for 4 to 6 weeks and a concomitant, usually gentle chemotherapy is given.
At the University Hospital Basel, we use the latest adaptive radiotherapy technology. Every day, we calculate a radiation plan that is precisely adapted to the anatomy in order to optimally target the tumor and spare the healthy organs.
Dr. A. Papachristofilou, Head of the Department of Radiation Oncology
System therapies for advanced bladder cancer
In the Oncology Department of the University Hospital Basel, we offer all system therapies for bladder cancer approved in Switzerland. We strive to give our patients these therapies in our outpatient clinic wherever possible, thus avoiding hospital stays.
In order to be able to offer innovative, new concepts in addition to the approved standard therapies, we are in constant contact with national and international study groups.
These study activities have, for example, enabled us to offer an "adjuvant", i.e. supportive, immunotherapy to reduce the risk of relapse after bladder surgery several years before approval in Switzerland (Checkmate-274 study, quote). None of our study patients had a relapse, and the feedback regarding this therapy was consistently positive.
The best possible therapy for your cancer
In addition to conventional chemotherapy, we also treat bladder cancer using immunotherapy and offer professional support with social and psychological issues.
Thanks to this wide range of services, we can assure our patients that we always offer state-of-the-art therapy and that we do everything we can to ensure that you receive the best possible treatment for your cancer.
Our offer also includes second opinions, for which you are welcome to register via the oncology office, for example in order to better understand your illness and the therapy concepts proposed to you.
Prof. F. Stenner, Deputy Head of Oncology
Registration for a second medical opinion:
Tel. +41 61 265 50 74
Tel. +41 61 265 50 59
or by e-mail onkologie@usb.ch
Molecular diagnostics: examination of cancer genes
An experienced team of pathology specialists assess urine cytology, tissue biopsies and surgical specimens.
In addition to a precise diagnosis of urinary tract tumors, biomarkers are determined on the tissue and cell material for the most tailored treatment possible using immunotherapy and targeted medication.
Prof. L. Bubendorf, Head Physician Pathology
Studies: Testing bladder cancer tissue in the laboratory
In order to better understand the biology of the disease, we allow the bladder cancer tissue to live on in the laboratory and can thus observe how cancer cells develop. This gives us the opportunity to test various drugs that can be used in patients.
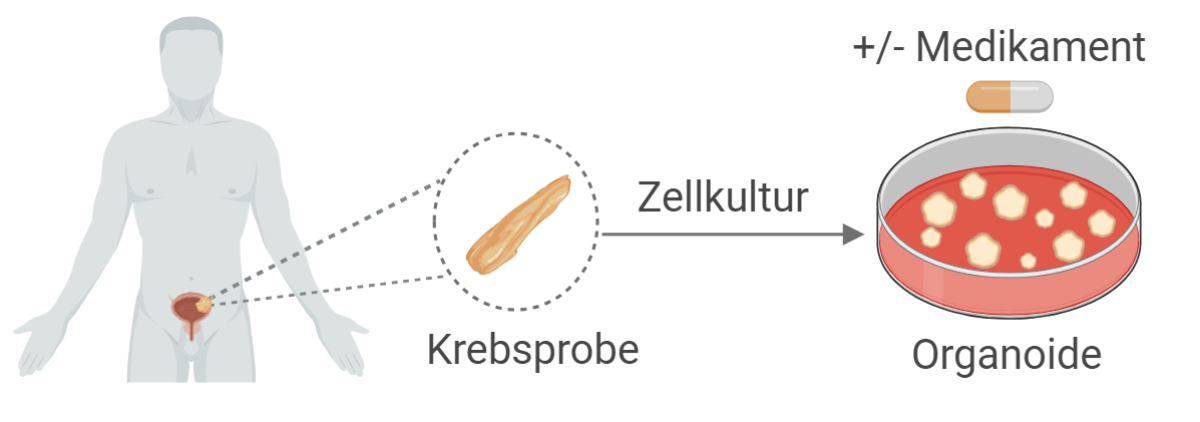
Generation of organoids derived from cancer samples of bladder cancer patients.
Illustration created by BioRender.com.
Our team is researching new ways to personalize the treatment of bladder cancer
In previous therapeutic approaches, patients with a certain type of cancer usually receive a similar treatment. However, it is becoming increasingly clear that this 'one-size-fits-all' approach is not always successful, and that while certain treatments work well for some patients, they do not show effective results for others.
To better understand the biology of the disease and personalize cancer treatment, we aim to keep bladder cancer tissue alive in the laboratory. These three-dimensional small cell clusters resemble 'mini' tumors of the respective patients. We also call these tumor cell clusters 'organoids'. We use these organoids as models or avatars to understand how cancer cells grow and develop and to test different drugs that could then be used. Overall, our research will ultimately help to find ways to improve and personalize the treatment of patients with bladder cancer.
Dr. C. Le Magnen, Research Group Leader Urology, Pathology, www.biomedizin.unibas.ch
Invasion assay with patient-derived organoid of sarcomatoid urethelial carcinoma (treated with DMSO, dimethyl sulfoxide).
These lab-grown organoids show us how cancer cells grow and develop.
Invasion assay with patient-derived organoid of sarcomatoid urethelial carcinoma (treated with dexamethasone, a steroid).
The growth of tumor organoids is prevented by treatment with glucocorticoids.
Interviews: What patients tell us
Read here what two male patients had to say about their experiences with bladder cancer and their treatment at the University Hospital Basel.
'Open discussions are important and help to deal with the illness'
Patient interview on the topic of the neobladder.
The interview was conducted by Anaïs Schlenker, December 2023
How did you realize that something was wrong? What symptoms did you experience?
I suddenly had blood in my urine, without any warning. Lots of blood and every time I urinated. I didn't have any pain, but it was a shock. That was in May 2021.
What was the path to diagnosis like?
My first appointment was with my GP. He referred me to a urologist, and the ultrasound examination was followed by a suspected diagnosis: several tumors in the bladder.
I was called in three times for tumor removal at Liestal Cantonal Hospital, where a transurethral resection of the bladder tumor was performed each time.
When the samples were taken, it was discovered that the tumor had already attacked the muscle tissue; as a result, further treatment options were discussed at an interdisciplinary tumor conference with a team of specialists from urology, oncology, radiotherapy and radiology.
Bladder tumors are usually diagnosed by cystoscopy, which is used to determine the indication for transurethral resection (removal of bladder tumors with an electrosurgical snare via the urethra) (Editor's note).
What treatment options were discussed with you at the University Hospital Basel?
I had my first appointment with PD Dr. Jan Ebbing at the Department of Urology at the University Hospital Basel in August 2021, accompanied by my wife.
It was explained to us that, in addition to chemotherapy, a complete removal of the bladder was necessary as the tumor had already grown into the muscles of the bladder.
Dr. Ebbing also discussed the various forms of urinary diversion with us (urinary stoma/conduit versus neobladder). We discussed the necessary requirements, the specific features of urinary diversion and the associated surgical risks.
I opted for the neoplasia. It was also decided that I would undergo chemotherapy first in order to be able to treat the tumor even better.
I was able to receive chemotherapy at Liestal Cantonal Hospital, for a total of four cycles. After the first cycle I still felt quite well, but after the second cycle I was struggling with skin rashes and exhaustion. And I was constantly cold. The freezing persisted and I still go to bed very early at night.
The neobladder surgery was performed successfully and without complications here at the USB by PD Dr. Jan Ebbing and Dr. Abolfazl Hosseini in January 2022.
The indication for chemotherapy is always individualized and patient- and tumor-specific. Side effects of chemotherapy occur and are discussed with the patient by the treating oncologists during the information session prior to treatment (editor's note).
How did the diagnosis affect you mentally? Who is supporting you?
A diagnosis like this turns everything upside down at first. You feel insecure and scared. But my family, my daughters, had greater difficulties accepting the diagnosis.
However, the most valuable and important thing is the support at home. I was informed about existing external support services, but I didn't want to take advantage of them. I am coping well.
At the USB, all tumor patients are psycho-oncologically evaluated and also receive psychological support on request (editor's note).
How did you feel after the bladder removal?
The pain was severe, but I'm good with pain. I was able to bear it. Mentally, you feel insecure and I also felt somehow at the mercy of others.
Pain can occur after bladder removal surgery, but there is good pain management. The minimally invasive approach and the use of robot-assisted keyhole surgery in particular significantly reduce the trauma to the body, which is associated with a faster recovery for patients and fewer complications (editor's note).
Later, after the bladder catheter was removed from the neobladder and the bladder filled with urine for the first time, I struggled with sleep deprivation. I had to set the alarm clock at night, first every two, then every three hours, so that there was no overloading with the new bladder. However, the accompanying pelvic floor therapy went well.
A neobladder has no sensitivity and no motor activity. The urine volume must first be trained. It is therefore normal for patients to initially have to empty their neobladder at night and set an alarm clock. Around 30% of male patients and 40% of female patients with a neobladder remain incontinent at night (more than 1 insert), whereas around 97% of male patients and around 75% of female patients are dry during the day (0 to a maximum of 1 insert per 24 hours), without restrictions (editor's note).
Would you make the same decision (for a neobubble) again?
Yes, it seemed like the best option for me right from the start.
How important is it to you to trust your doctor? Do you feel that you are in good hands?
I always felt well supported and looked after here at the University Hospital Basel.
How are you feeling today? Are there any restrictions in your everyday life?
I was able to return to work in May 2022. Everything works well during the day and I have no problems or complications. At night (when my head isn't thinking) I have to wear insoles. I no longer have to take any medication. With the exception of erection support.
If the tumor situation allows, the erectile nerves, or the nerves for sexual stimulation, can be spared during bladder removal so that sexual function is maintained after a rehabilitation phase. However, additional medication may be necessary to support the erection (editor's note).
What happens next?
I am called in for a check-up every six months and then once a year. So far, everything has been normal.
The follow-up intervals depend on the patient's tumor situation and the current guidelines of the specialist associations, such as the European Association of Urology (EAU) (editor's note).
What would you like to give other patients?
Communicate openly with family and friends. I felt the need to spare my loved ones and family, but open conversations were the best way to help everyone deal with the illness.
Even with work colleagues and acquaintances, there were those who avoided me and those who asked directly how I was doing. I was able to give a direct answer, and that was always really good.
'I want to show my body that I'm not giving up'
Patient interview on the topic of bladder tumors and instillation.
The interview was conducted by Anaïs Schlenker, December 2023
How did you realize that something was wrong? What symptoms did you experience?
It all started with a painful hip in the fall of 2022, when I was in the USA on business. I came back to Switzerland and had to undergo hip surgery in December. Following the operation, blood was found in my urine, a typical symptom of bladder cancer.
What was it like to be diagnosed and how did you feel after the operation?
The diagnosis after the CT confirmed the suspicion of a bladder tumor. I was unable to return to the USA, and I am still unable to work regularly. However, this is only partly due to the bladder tumor and the associated treatment.
In January 2023, I had my first operation in a Basel hospital outside the USB. The first TUR-B (transurethral resection of bladder tissue) was followed by a resection.
In March, a BCG (Bacillus Calmette-Guérin) instillation into the bladder was started there. After the third instillation, my knee and calf swelled up. A side effect of the instillation that was not recognized as such. This was followed by an operation on my knee and a puncture in my hip. The BCG therapy had to be discontinued.
Three small tumors were discovered during a cystoscopy at the end of May. Two tumors were superficial, one tumor turned out to be a carcinoma in situ (CIS) with a high risk of recurrence.
How did the diagnosis affect you mentally? Who is supporting you?
This marathon of doctors and diagnoses is extremely stressful and tiring. My daughter accompanied me to the appointments a few times. Of course, you also try to gather information yourself via all available channels.
I also sought external psychological help. But only for a short time. Ultimately, you have to deal with the illness on your own. I also try not to burden my family too much with it.
I also had to learn that the emotional life during such treatment is not so easy to explain and that you shouldn't underestimate the psychological strain.
When were you referred to the University Hospital Basel?
After the second TUR-B, I received a first instillation of epirubicin at an external hospital. This is the standard therapy.
In August 2023, a referral to Prof. Cyrill Rentsch at the University Hospital Basel was discussed at the external tumor board. Here at the Urology Clinic, a local gemcitabine/docetaxel combination therapy is offered , which is more promising than epirubicin. The therapy was then started immediately.
How often do you come to our clinic?
The procedure for the instillation cycle was as follows: For six weeks, I received alternating doses of chemotherapy flushed into the urinary bladder on two consecutive days. On the first day a dose of gemcitabine, on the following day a dose of docetaxel. This was followed by a four-week break.
Subsequently, after a cystoscopy without new evidence of cancer, monthly maintenance therapy was started.
We had the first consultation after the appointment for the last round of instillations. The patient appears athletic, open, composed, but also tired. This is one of the side effects that he struggles with in the first 3-5 days after instillation. Exhaustion and nightmares also bother him.
Do you feel you are in good hands with us?
After many visits to the doctor and stays in various hospitals, I had to readjust to the University Hospital Basel. The USB is a big place, so you can feel like one of many. But the priority is to get the right treatment. This is the case here.
I feel that I am in good hands with my attending physician, Prof. Cyrill Rentsch. My thanks also go to Heike Püschel, Study Nurse, who looks after me with great empathy during every examination. This is extremely valuable.
What happens next?
I am currently on maintenance treatment. For 12 months, I come to the clinic every month on two consecutive days and receive a dose of Gemcitabine on the first day and a dose of Docetaxel on the second day.
To date, the findings are: no visible tumors.
What would you like to give other patients?
For me, it's important to feel my body and keep moving. In my case, swimming and running training sessions helped me a lot to forget about the tumor, at least temporarily.
That's what I would say to someone living with a similar diagnosis - don't let up, fight. And believe in yourself.
Brochures for patients on the subject of bladder cancer
We recommend the information brochures "Bladder Cancer" and "The Urostomy" from the Swiss Cancer League. There you will find further useful information on the subject.

Frequently asked questions

What increases the risk of bladder cancer?
The main risk factor for bladder cancer is smoking. Stopping smoking can have a positive effect on the relapse and progression of bladder cancer . Read more about our stop smoking consultation at the USB.
What are the symptoms?
The first signs are pain when urinating and frequent urination. However, the main symptom is visible or non-visible, painless blood loss in the urine. Patients with these symptoms should definitely be seen by a urologist.
Suspected bladder cancer - What happens next?
If bladder cancer is suspected, we will perform a cystoscopy. Nowadays, this procedure can be performed on an outpatient basis and without anesthesia during consultation hours thanks to the use of a flexible camera. A cystoscopy only takes a few minutes. We will also perform a bladder irrigation to examine whether malignant bladder mucosa cells can be found. If these examinations reveal any abnormalities, a tissue sample is taken from the bladder through the urethra in a minimally invasive procedure without a skin incision.
What forms of therapy are available?
If a bladder tumor is found in the cystoscopy, it is removed through the urethra under anaesthetic. When first diagnosed, most bladder tumors are limited to the mucous membrane (70%) and the bladder can be preserved.
Urinary bladder tumors limited to the mucous membrane have a high risk of recurrence. To reduce this risk, after removal of the tumors, medication is injected into the bladder via the urethra at regular intervals using a catheter to reduce the risk of recurrence. Read more about our instillation therapy.
If the cancer has already grown into the muscles of the bladder when it is first diagnosed, the bladder must be surgically removed or treated with radiotherapy and chemotherapy.
Read more about robot-assisted cystectomy, radiotherapy and chemotherapy.
If the bladder is completely removed, urine can no longer be excreted naturally via the urethra. A replacement for urine drainage from the kidneys is created.
In rare cases, however, bladder cancer has already spread throughout the body. In this case, cure by surgery and radiotherapy is no longer likely. However, there are good therapies that can greatly prevent further progression of the disease.
What are the chances of recovery?
The earlier bladder cancer is detected, the higher the chances of recovery. In many cases, the entire bladder cancer can be removed with a tissue sample via the urethra. If the tumor has not yet grown into the muscle layer of the bladder, the chances of recovery are around 80%.
Depending on how deep the cancer has penetrated into the bladder wall and how malignant it is, it may be necessary to remove more of the bladder mucosa.
Can bladder cancer return?
Unfortunately, non-muscle-invasive bladder cancer often returns even after complete removal.
Our clinic has extensive experience in advanced bladder tumor therapy. BCG immunotherapy (Bacillus Calmette-Guérin) can significantly reduce the likelihood of bladder tumors returning. We are actively conducting research in the field of BCG immunotherapy and are supported by the Swiss Group for Clinical Cancer Research (SAKK).
We offer our patients individual tumor follow-up care in order to detect bladder tumor recurrences at an early stage and treat them accordingly.
Approach & Contact
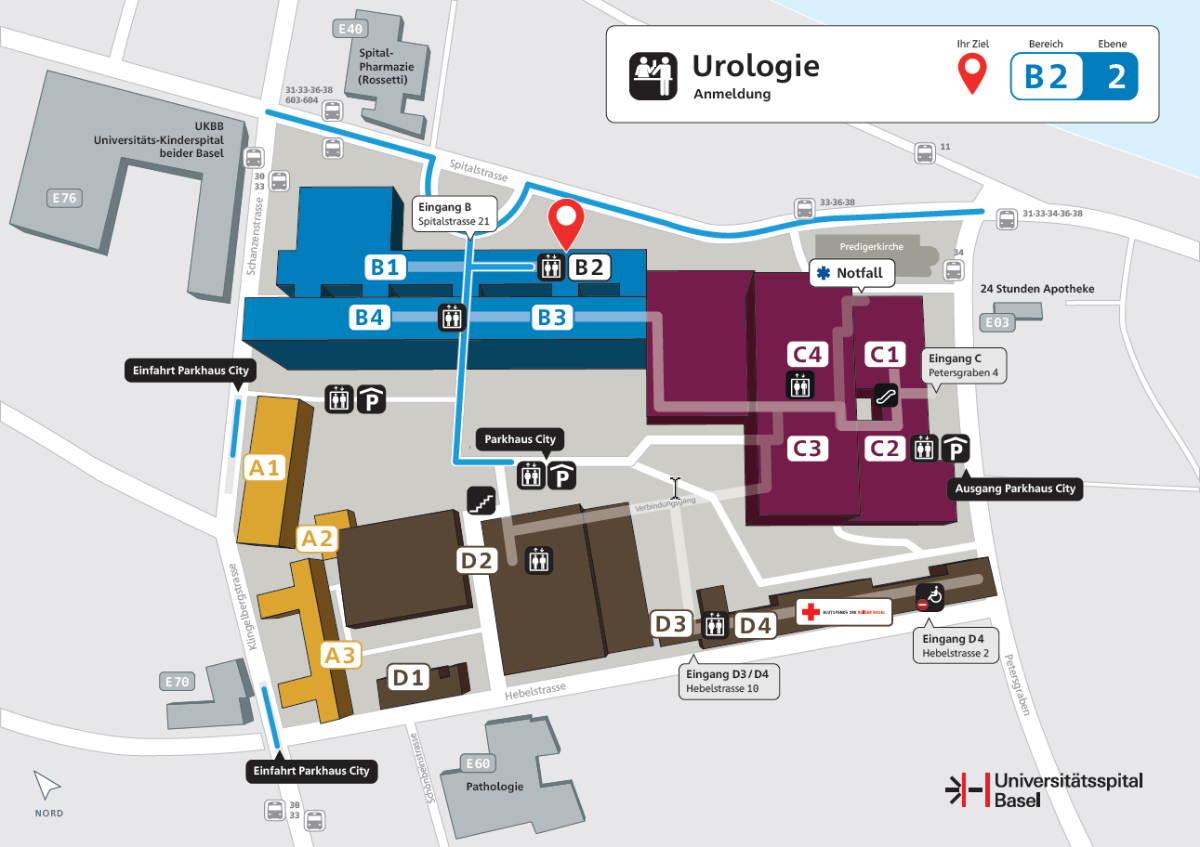
Address
|
University Hospital Basel |
By streetcar
| Take streetcar line 11 to the University Hospital station and then follow Spitalstrasse on foot for about 250m to the entrance. |
By car
| Please use the parking garage City, entrance Schanzenstrasse or Klingelbergstrasse. |
Contact us
Urology registration office
Availability: Mon-Fri, 08.00 - 16.00 hrs
Phone +41 61 265 72 80
anmeldung.urologie@usb.ch
Contact for emergencies
During operating hours, please contact the Urology Registration Office. For urological emergencies outside of operating hours, the Emergency Center at the USB is there for you around the clock:
Emergency Center University Hospital Basel
Petersgraben 2
4031 Basel
Phone +41 61 265 25 25
Contact for queries about your operation
Surgery Coordination Urology
Phone +41 61 328 58 15
op.urologie@usb.ch


