
Research
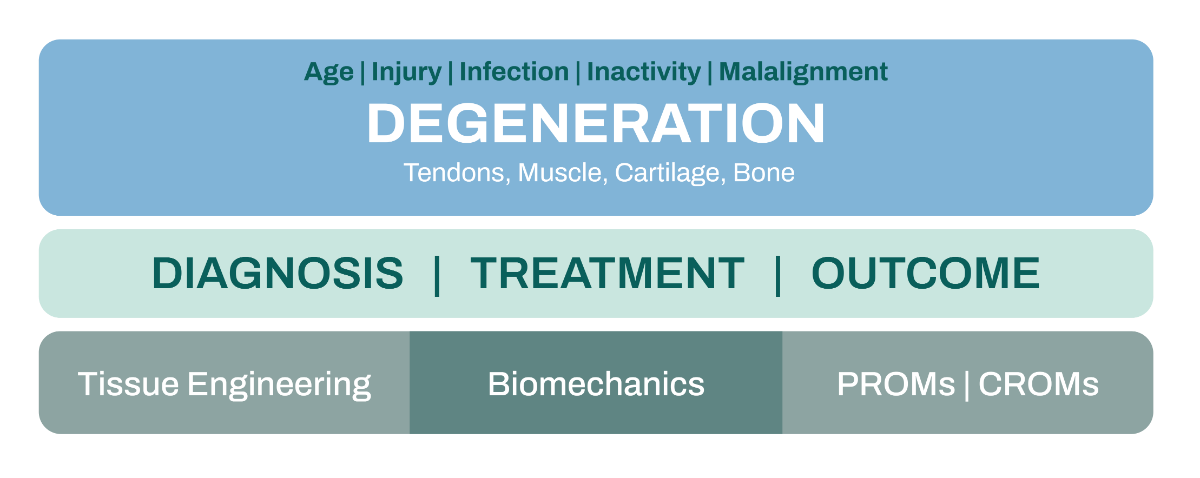
Unsere Klinik forscht auf nationaler und internationaler Ebene. Die Forschung gliedert sich in Grundlagenforschung (Biomechanik, muskuloskelettale Modellierung, Tissue Engineering) und klinisch-translationale Forschung (Behandlungsstrategien). Der Schwerpunkt liegt auf der Erforschung der Degeneration von Gewebe (Muskeln, Sehnen, Knochen und Knorpel) aufgrund von Verletzungen, Fehlstellungen, Infektionen oder Alter.
Unser Ziel ist es, die Genauigkeit und Effizienz von Diagnosen mithilfe von KI- und Sensortechnologien, fortschrittlicher Bildgebung und Gewebe-Biomarkern für Erkrankungen des Bewegungsapparats zu verbessern und die Präzision, Personalisierung und Wirksamkeit therapeutischer Massnahmen für Patienten mit degenerativen muskuloskelettalen Erkrankungen und Verletzungen zu erhöhen.
Orthopaedics and Traumatology Research
The Clinic for Orthopaedics and Traumatology has a national and international presence in orthopaedic research that is based on a broad representation of the various subspecialties within this surgical field. Our faculty members are dedicated to development of novel surgical modalities and therapeutic concepts by conducting translational medicine that bridges basic science and clinical practice. We aim to create a rich research environment by promoting active, multidisciplinary cooperation among orthopaedic surgeons, radiologists, engineers, movement scientists, study nurses, biostatisticians and physiotherapists and collaborations with other centers. Fundamental to our research endeavor is providing a stimulating educational environment for students, orthopaedic registrars and researchers. Research at our clinic is organized in the focus areas tissue engineering, clinical research and functional biomechanics.

Dr. Marlene Mauch
Leiterin Research Management Outcome Research
Orthopädie und Traumatologie
Orthopaedics and Traumatology Research
Das Scientific Advisory Board (SAB) der Orthopädie und Traumatologie koordiniert die wissenschaftlichen Aktivitäten im Sinne der Forschungsstrategie. Das SAB ist interdisziplinär mit Vertreter:innen der universitären Partnerinstitute sowie der klinischen Forschung, der biomechanischen Forschung und des Forschungsmanagements zusammengesetzt.
Vorsitz

Prof. Andreas Marc Müller
Chefarzt
Orthopädie und Traumatologie
Leiter Team Schulter / Ellenbogen
Forschungsschwerpunkte
Schulter und Ellbogen
Im Bereich der Schulter- und Ellenbogenforschung stehen aktuell drei Schwerpunkte im Fokus:
Prothetik-Forschung
Ein zentraler Bestandteil dieses Forschungsschwerpunkts ist die Implementierung eines prospektiven, multizentrischen Schulterprothesen-Registers. Ein solches Register ermöglicht eine systematische Analyse der verwendeten Implantaten, Operationstechniken sowie der Langzeitergebnisse und Komplikationen nach Implantation von Schulterprothesen. Ziel ist es, evidenzbasierte Empfehlungen zur optimalen Patientenversorgung mit Schulterprothesen abzuleiten und die Versorgungsqualität und Sicherheit weiter zu verbessern.
Rotatorenmanschettenrupturen
Ein weiterer Schwerpunkt liegt auf der Erforschung des Sehnenmetabolismus und der Sehnenheilung bei Rupturen und degenerativen Veränderungen der Rotatorenmanschette. Dabei werden biologische Prozesse und neue therapeutische Ansätze zur Regeneration und Heilung der Sehnen untersucht. Die Erkenntnisse aus dieser Forschung sollen dazu beitragen, die Behandlungsergebnisse bei Läsionen der Rotatorenmanschette zu optimieren um die Funktionalität der Schulter langfristig zu erhalten.
Innovative Knorpelregeneration am Schulter- und Ellbogengelenk
Durch interdisziplinäre Kooperation können wir experimentelle und innovative Methoden zur Knorpel Knorpelregeneration am Schulter- und Ellbogengelenk entwickeln, anbieten und klinisch erforschen. Durch Transplantation von Nasenknorpel ins Schulter- und Ellbogengelenk (nose-to-shoulder, nose-to-elbow) können wir auch fortgeschrittene Knorpelschäden regenerieren um das native Gelenk langfristig zu erhalten.

Prof. Andreas Marc Müller
Chefarzt
Orthopädie und Traumatologie
Leiter Team Schulter / Ellenbogen
Prof. Dirk Maier
Leitender Arzt / Standortleiter Bethesda
Orthopädie und Traumatologie
Stv. Teamleitung Schulter/Ellbogenorthopädie
Hüfte und Becken
Der zentrale Fokus unserer Forschung liegt im Bereich der Hüft-Endoprothetik. Ein besonderer Schwerpunkt liegt dabei auf der Analyse von Implantatmigration, um die Langzeitstabilität und Funktionalität von Hüftprothesen besser beurteilen zu können. Ein weiteres Ziel ist es, die Ätiologie und optimale Behandlungsstrategien bei periprothetischen Frakturen zu verstehen und weiterzuentwickeln.

Prof. Karl Stoffel
Stv. Chefarzt
Orthopädie und Traumatologie
Leiter Team Traumatologie / Team Hüfte und Becken
Knie- und Sportorthopädie
Knorpelprojekte «Encanto» und «PFOA-II»
Die Encanto Studie ist eine randomisierte, kontrollierte, multizentrische klinische Phase-II-Studie zur Behandlung der patellofemoralen Arthrose mit Implantation von Knorpelgewebe auf der Basis nasaler Chondrozyten im Vergleich zur derzeitigen Standardbehandlung.
Bei einer Kniescheibenarthrose stehen Physiotherapie, Injektionen von Hyaluronsäure oder plättchenreichem Plasma aus Eigenblut oder ein künstlicher Gelenkersatz mit einer (Teil-) Knieprothese als Standardtherapie zur Verfügung. Damit soll eine Linderung der Schmerzen und eine bessere Funktion des Knies erreicht werden.
In dieser Studie untersuchen wir, wie die Prüfsubstanz N-TEC bei der Behandlung der Knie-scheibenarthrose wirkt und ob sie wirksam und gut verträglich ist.
In der PFOA-II Studie vergleichen wir aktuell die Wirksamkeit der autologen Membran im Vergleich zu der PRP-Infiltration.
Kreuzbandprojekt
Prospektive Untersuchungen der ligamentären Chirurgie an Kreuzbändern des Kniegelenkes mit deren Revisionen und Folgeschäden.
Es wird eine multizentrische schweizweite Erhebung von Re-Rupturen der Kreuzbandplastiken und Rekonstruktionen durchgeführt, um prognostische Faktoren auf das Versagen der heutigen Standardtherapien zu eruieren und bessere Vorhersagemodelle zu entwickeln. Es werden daraus Behandlungsalgorithmen für die Revisionschirurgie bei erneuten Kreuzband- und Meniskus-Operationen generiert.
Prothetik-Forschung
Der künstliche Kniegelenksersatz zählt zu den häufigsten orthopädischen Eingriffen. Der Erfolg hängt jedoch von vielen Faktoren ab – darunter Operationstechnik, Implantatdesign, Muskelfunktion und Rehabilitation. Entscheidend für die Patient:innen ist jedoch vor allem eines: Wie gut funktioniert das Gelenk im Alltag?
Unsere Forschung im Bereich der Knieprothetik – aktuell unter anderem im Rahmen der Projekte TEPstabil und CAT – verbindet modernste biomechanische Analysen mit patientenzentrierten Ergebnismessungen.
Was untersuchen wir konkret?
- Technische Validierung radiologischer Messmethoden, um die Genauigkeit und Zuverlässigkeit der Prothesenpositionierung sicherzustellen
- Zusammenhänge zwischen Prothesen-Alignment und klinischem Outcome, z. B. Schmerzfreiheit, Stabilität und Patientenzufriedenheit
- Biomechanische Ganganalysen, um zu verstehen, wie das Implantat die Funktion bei unterschiedlichen Alltagsaktivitäten beeinflusst (sog. funktionelle Biomechanik)
Dabei stehen Patient-Reported Outcome Measures (PROMs) ebenso im Fokus wie objektive Bewegungsdaten. Unser Ziel ist es, nicht nur das Röntgenbild zu verbessern, sondern vor allem die Lebensqualität unserer Patient:innen nachhaltig zu steigern.
Alle Prozesse betreffend Knieprothetik finden nach den neuesten wissenschaftlichen Standards und unter streng kontrollierten Qualitätskriterien als Teil unseres zertifizierten Endoprothetikzentrum statt (Hier link zur Prothetikzentrum)
Kontakt und Anfragen: knie-team@usb.ch

PD Dr. Petros Ismailidis
Kaderarzt / Leiter Endoprothetikzentrum
Orthopädie und Traumatologie
Zentrum für muskuloskelettale Infektionen (ZMSI)
Fuss und Sprunggelenk
Via «Statistical Shape Modeling» entwickeln wir im Bereich Fuss- und Sprunggelenk Modelle für eine bessere Beurteilung von Abnützungen der Gelenke (Arthrose) und Fehlstellungen (Deformitäten). Der Fokus liegt insbesondere auf der Entwicklung einer patientenspezifischen Behandlung der oberen Sprunggelenkarthrose.

PD Dr. Nicola Krähenbühl
Leitender Arzt
Orthopädie und Traumatologie
Leiter Team Fuss und Sprunggelenk
Zentrum für muskuloskelettale Infektionen
Das Zentrum für muskuloskelettale Infektionen (ZMSI) widmet sich der interdisziplinären Forschung und klinischen Innovation im Bereich komplexer Infektionen des Bewegungsapparats. Ziel ist es, durch translationales Arbeiten neue diagnostische und therapeutische Ansätze zu entwickeln und die Versorgung von Patient:innen mit muskuloskelettalen Infektionen nachhaltig zu verbessern.
Forschungsschwerpunkte:
- Prothesenassoziierte Infektionen und innovative Versorgungskonzepte.
- Fraktur-assoziierte Infektionen
- Knochendefekte und Pseudarthrosen
- 3D Printing, Navigation
- Infektionen periprothetischer Frakturen
Kollaborationen:
Kollaboration mit dem NCCR Antiresist – Bakterielle Physiologie bei muskuloskelettalen Infektionen: https://www.nccr-antiresist.ch/de/

Prof. Martin Clauss
Stv. Chefarzt / Standortleiter Universitätsspital Basel
Orthopädie und Traumatologie
Leiter Zentrum für muskuloskelettale Infektionen (ZMSI)

PD Dr. Mario Morgenstern
Leitender Arzt, Leiter Klinische Forschung
Orthopädie und Traumatologie
Stv. Leiter Zentrum für muskuloskelettale Infektionen (ZMSI)
Trauma und Polytrauma
Traumatologie
Unser Team erforscht Frakturen der oberen und unteren Extremität, mit besonderem Fokus auf proximale und distale Radiusfrakturen sowie proximale Humerusfrakturen. Ziel ist die Bewertung von Behandlungspfaden, mittel- und langfristigen Ergebnissen sowie bild- und scorebasierten Entscheidungshilfen. Ergänzend entwickeln wir KI-gestützte Algorithmen zur automatisierten Frakturklassifikation.

Prof. Karl Stoffel
Stv. Chefarzt
Orthopädie und Traumatologie
Leiter Team Traumatologie / Team Hüfte und Becken

Dr. Birgit Oberreiter
Kaderärztin / Stv. Teamleitung Trauma
Orthopädie und Traumatologie
Polytrauma
Wir untersuchen mikrobiologische und klinische Veränderungen bei Kombinationsverletzungen und betreiben klinische Outcomeforschung im Kontext der Versorgung Schwerverletzter, um die Behandlungsqualität und Prognose nachhaltig zu verbessern.

Alterstraumazentrum
Ein Schwerpunkt unserer Forschung liegt auf der intraoperativen Bildgebung bei Frakturen, insbesondere bei pertrochantären Femurfrakturen und distalen Radiusfrakturen. Dabei vergleichen wir die Effizienz des robotergesteuerten CIARTIC Move mit dem nicht motorisierten CIOS Spin. Als Frakturmodelle dienen die bildgeführte Marknagelosteosynthese mit TFNA sowie die Plattenosteosynthese.
Im Bereich der orthogeriatrischen Versorgung untersuchen wir Fragilitätsfrakturen und entwickeln strukturierte Behandlungspfade. Dazu gehören retrospektive und prospektive Analysen bildgeführter Eingriffe am Beckenring.
Parallel dazu sind wir an mehreren vorklinischen Projekten beteiligt, unter anderem zur Metallartefaktreduktion und zur Rotationsbestimmung nach Marknagelosteosynthesen bei Schaftfrakturen.

Prof. Norbert Suhm
Leitender Arzt/Zentrumsleiter Alterstraumazentrum
Orthopädie und Traumatologie
Leiter Alterstraumazentrum
Biomechanische Forschung
Im Labor für Funktionelle Biomechanik erfassen wir Bewegungen, Gelenksfunktionen und Muskelaktivität mithilfe modernster dreidimensionaler Bewegungsanalyse. Unser Ziel ist es, funktionelle Einschränkungen, Fehlbelastungen und muskuläre Dysbalancen bei degenerativen Erkrankungen und Verletzungen des Bewegungsapparates (z. B. Knie, Schulter, Wirbelsäule) sichtbar zu machen und so eine gezielte Therapie zu ermöglichen.
Unsere Forschungsschwerpunkte:
- Mobile Bewegungsanalyse: Einsatz von Inertialsensoren (IMUs), die direkt am Patienten angebracht werden, um Gangbild und funktionelle Bewegungen in der klinischen Routine präzise zu erfassen (z.B. in der Prothetik-Forschung)
- Schulterfunktion nach Rotatorenmanschettenverletzungen: Analyse der Gelenks- und Muskelaktivität bei alltagsrelevanten Bewegungen zur Optimierung von Therapie und Rehabilitation (siehe Schulterforschung)
Durch diese dynamische Beurteilung von Bewegungsmustern leisten wir einen wichtigen Beitrag zur personalisierten orthopädischen Versorgung.

Dr. Corina Nüesch
Leiterin Labor für Funktionelle Biomechanik / Leiterin Forschung Spinale Biomechanik
Orthopädie und Traumatologie / Spinale Chirurgie

Wir forschen mit folgenden Instituten der Universität Basel:
Department of Biomedicine (DBM)
Das übergeordnete Ziel der Tissue Engineering-Gruppe ist die Entwicklung zellbasierter Transplantate zur Reparatur von Knorpel- und Knochengewebe sowie komplexer osteochondraler Läsionen. Über die potenzielle klinische Anwendung als Implantate hinaus dienen die konstruierten Gewebe auch als wertvolle 3D-Modellsysteme zur Untersuchung der Differenzierung von Vorläuferzellen und der Gewebeentwicklung.
Die zentralen wissenschaftlichen Fragestellungen betreffen:
- Die Funktionalität menschlicher mesenchymaler Zellen (reife Zellen, Vorläuferzellen, Stammzellen) für die Reparatur von Knochen und Knorpel.
- Den Einfluss spezifischer chemischer und physikalischer Umweltfaktoren auf das Tissue Engineering des Skelettsystems.
- Die Interaktion verschiedener Zelltypen während der ex vivo-Gewebemorphogenese.
Die Projekte bewegen sich an der Schnittstelle zwischen Grundlagenforschung und klinischer Anwendung und vereinen die Expertise von Biolog:innen, Ingenieur:innen und Chirurg:innen.
Neben nationalen Förderprogrammen (z. B. SNF) und industriellen Kooperationen wird die Forschung auch im Rahmen europäischer Konsortien unterstützt, was eine starke internationale Vernetzung der Gruppe begünstigt.


Department of Biomedical Engineering (DBE)
Die Biomechanik widmet sich der Komplexität des menschlichen Körpers und seiner Funktion. Wir erforschen die Zusammenhänge zwischen Struktur und Funktion sowie die Entstehung, den Verlauf und die Behandlung orthopädischer Erkrankungen (z. B. Arthrose) und Verletzungen (z. B. Frakturen). Wissenschaftler:innen und Kliniker:innen arbeiten interdisziplinär zusammen, um klinisch relevante Erkenntnisse zu gewinnen und die bestmögliche Funktion nach Erkrankung, Verletzung oder Gelenkersatz zu erhalten oder wiederherzustellen.
Research | Department of Biomedical Engineering | University of Basel

Prof. Philippe Claude Cattin
Head of DBE
Center for medical Image Analysis and Navigation (CIAN)

Klinische Forschung (SORC/ DKF)
Das Surgical Outcome Research Center (SORC) und das Department Klinische Forschung unterstützen die Klinik für Orthopädie und Traumatologie bei der Initiierung und Umsetzung multizentrischer Forschungsprojekte sowie beim Aufbau klinischer Register. Der umfassende Support erleichtert die Durchführung qualitativ hochwertiger klinischer Forschung und fördert die effiziente Umsetzung innovativer Studienkonzepte.
Unsere Publikationen
