Offer
Our clinic offers its patients the complete spectrum of oral and maxillofacial surgery, including plastic surgery in the facial area. It includes traumatology of the facial skull, tumor surgery with aesthetic and masticatory rehabilitation, treatment of cleft lip and palate, treatment of jaw malpositions and craniofacial anomalies using the latest 3D planning and navigation technology, skull base and orbital surgery, treatment of temporomandibular joint disorders, as well as implantology and pre-prosthetic surgery.
In the head and neck area, various organ systems (brain, eyes, ears) are in close proximity and are often affected in combination by diseases and injuries. This makes interdisciplinary cooperation with neighboring disciplines (e.g. neurosurgery, ENT, dentistry) in diagnostics and therapy an essential element of the specialty. Together with the ENT Clinic, we look after the Center for Head, Neck and Eye Tumors at the University Hospital Basel. Pediatricians, orthodontists, ENT specialists and speech therapists work together in our interdisciplinary cleft center.
Emergencies
Phone +41 61 265 70 70
(Clinic secretariat)
Dysgnathie - Was ist das?
Dysgnathie - Der Behandlungsablauf
Dysgnathie - Die Operation und die Nachsorge
Notes for emergencies
What should be done in maxillofacial surgery emergencies?
So that we can assess your problem and offer you an appointment as quickly as possible, please contact our clinic secretariat by telephone:
Tel. +41 61 265 70 70.
Outside our opening hours or in urgent emergencies, please present yourself at the interdisciplinary emergency ward of the University Hospital Basel, Petersgraben 4.
We have an oral and maxillofacial surgeon on call around the clock, 7 days a week, who will be available to attend to you in an emergency.
If you already have a doctor's letter/referral letter, x-rays or other medical documents, please bring these with you to your appointment.
Our range of services at a glance
Jaw fractures / traumatology of the facial skull
As an exposed part of the body, the head is at particularly high risk of injury. The team at the Department of Oral and Maxillofacial Surgery treats dental injuries, injuries to the soft tissues of the face, as well as fractures of the bones of the facial skull and even serious and severe injuries as part of a polytrauma. Injured persons are usually admitted via the emergency ward of the university hospital, from where the oral and maxillofacial surgeon is called in. In special situations, patients can also contact the doctor on duty via the University Hospital switchboard
Tel. +41 61 265 25 25.
In the treatment of fractures of the facial skull, the usual techniques of internal fixation of the bone are used. This technique allows the fractured bone fragments to be positioned perfectly without causing any significant impairment to the patient. The healing time is usually quite short. Minimally invasive surgical procedures are also used, which also contribute to a short hospital stay.
Once inpatient treatment has been completed, affected patients continue to receive outpatient care in the injury consultation hours. Appointments can be made via the clinic secretariat
Tel. +41 61 265 70 70, Fax. +41 61 265 70 71.
Tumor surgery with aesthetic / masticatory rehabilitation
Malignant tumors in the oral and maxillofacial region - especially of the oral mucosa - are the sixth most common tumor disease worldwide and are on the rise.
At the University Hospital Basel, patients affected by malignant tumors in the head and neck area benefit from interdisciplinary care at a high university level. From diagnosis to rehabilitation, the interdisciplinary Head and Neck Tumor Center involves specialists from the Clinics of Oral and Maxillofacial Surgery, Otorhinolaryngology and the Institute of Radio-Oncology, the Department of Oncology, the Institute of Diagnostic Radiology, the Clinic of Dental Surgery and the Institute of Pathology.
The formation of the center does not mean that patients now have to enter an anonymous cancer center. In future, patients will continue to be cared for personally by their doctor throughout their treatment. Patients and their relatives will continue to have personal discussions with these caregivers. All patients are now regularly presented to an interdisciplinary committee of specialists from the above-mentioned fields. In each case, they decide together on the best therapy.
After surgical treatment, patients are regularly followed up under the supervision of senior physicians. All measures for functional and aesthetic rehabilitation are initiated and carried out as part of the follow-up care. Patients concerned can make an appointment with the senior consultants via the clinic secretary's office, or arrange for a referral directly from their family doctor or dentist
Tel. +41 61 265 70 70, Fax. +41 61 265 70 71.
Cleft lip and palate
Cleft lip and palate is the most common congenital malformation of the jaw and face and affects around one in 700 newborns. This change occurs between the 6th and 12th week of development because the lip and palate halves of both sides do not unite. In most cases, however, the rest of the child's development proceeds completely normally. The fusion of the lip and palate halves must therefore be made up for after birth by an operation to allow the nose and mouth to function normally. In the case of unilateral clefts, this is done in one operation in the first year of life, in the case of bilateral cleft lip and palate, sometimes in two stages. The concept of "one-stage" closure has existed in Basel since 1991 and has been further developed several times according to the latest medical findings.
Depending on the type of cleft and the age of the child, different specialists are required for the treatment. In the university treatment network for cleft lip and palate, we bring specialists together for you. Several specialists are therefore present at the same time in the special consultation hours. This means that treatment decisions can be discussed and determined directly. This reduces the stress for the child and parents to the bare minimum and treatment steps can be optimally coordinated. This form of interdisciplinary consultation has been practiced in Basel for over 30 years.
Further information on the topics listed below can be found on the website of the Center for Cleft Lip and Palate:
- Manifestations (DE/EN/FR)
- Concomitant symptoms and consequences (DE/EN/FR)
- Diagnosis and treatment (DE/EN/FR)
- Further measures (DE/EN/FR)
- Speech therapy - Function-oriented speech therapy
- Research and publications
Appointments, patient coordination & nursing advice
We will be happy to advise you individually and answer your questions personally. Please make an appointment(+41 61 328 73 47, Mon/Thu) or call us directly for information(+41 61 328 60 95).
Anita Lukic
Special Nurs
eResource Nursing Specialist Development
Appointments Monday and Thursday under:
Email daily anita.lukic@usb.ch
For administrative matters
Hümeyra Yagci
Secretariat
Prof. Dr. med. Dr. med. dent. Müller
Further links
Jaw malpositions / dysgnathia
Malpositions or positional anomalies of the jaws, known as dysgnathia, can affect the external appearance (aesthetics), but can also lead to a number of sometimes serious functional problems. For example, if the upper or lower jaw protrudes or recedes too far, the rows of teeth do not fit together properly. This can cause discomfort when eating and speaking. Lip closure is often not possible. The chewing muscles as well as the muscles of the neck can react with tension. Temporomandibular joint problems can be the result. Inadequate loading of the teeth can lead to their premature loss. The creation of an ideal chewing and swallowing function while at the same time optimizing the patient's external appearance is therefore at the forefront of treatment planning and implementation.
The treatment of affected patients is carried out by the oral and maxillofacial surgeon in close coordination with the orthodontist in charge, who is responsible for adjusting the position of the teeth. Close consultation between the specialists is essential for the success of the treatment. For this reason, regular interdisciplinary dysgnathia consultations are held at our clinic, where patients are seen by both doctors at the same time.
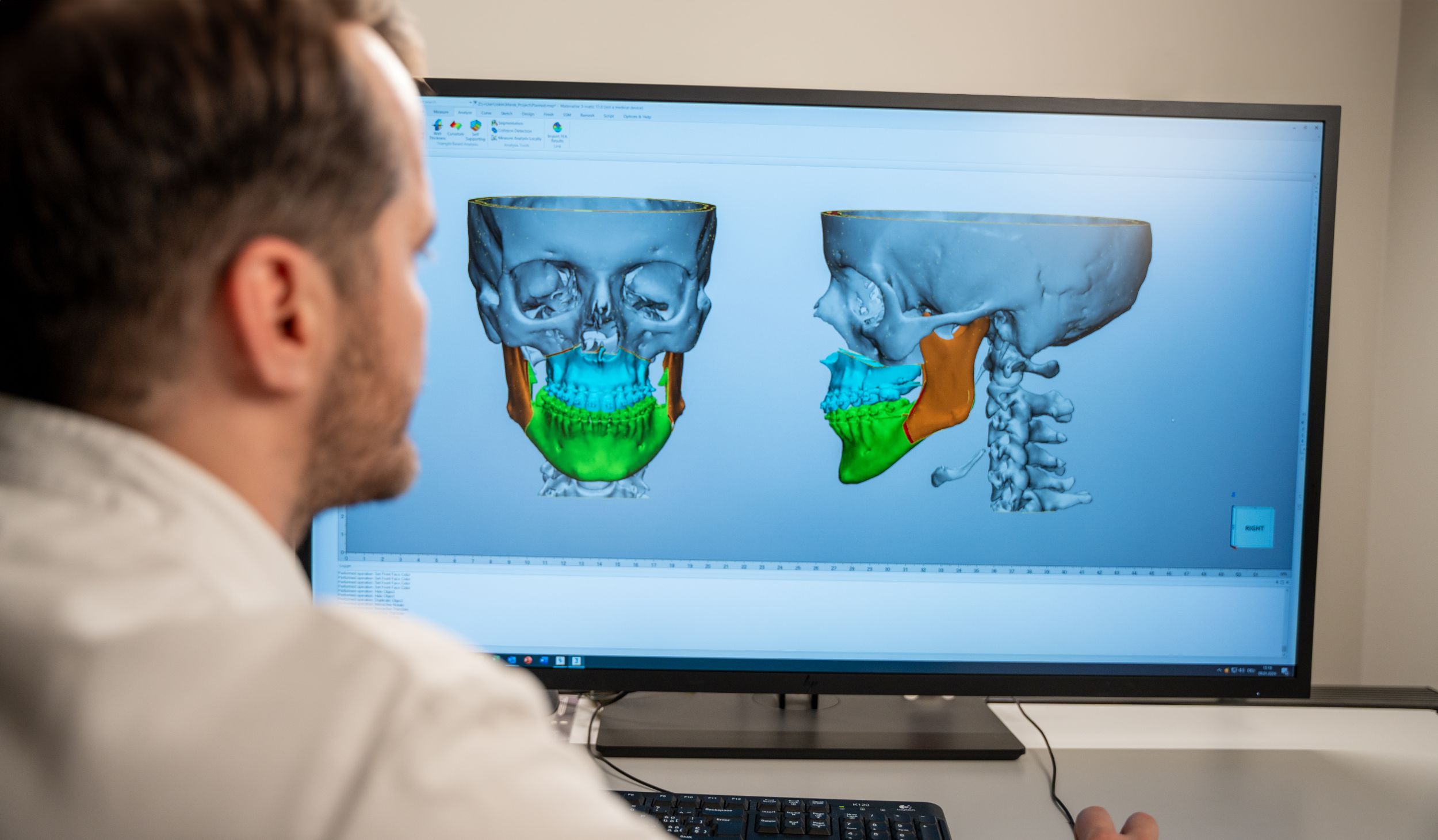
State-of-the-art technologies are used for surgical planning. The surgical repositioning of the jaws is routinely planned in three dimensions. This allows the patient to be shown approximately how their external appearance will change as a result of the operation even before the operation.
Affected patients can make an appointment for the "Dysgnathia consultation" directly via the clinic secretary's office, or arrange a referral through the treating orthodontist
Tel. +41 61 265 70 70, Fax. +41 61 265 70 71
Temporomandibular joint disorders
Disorders of the temporomandibular joint and discomfort in the masticatory muscles can have different causes. In most cases, pain is caused by a malfunction of the temporomandibular joint. These dysfunctions can be caused by a disorder of the muscles that move the lower jaw, but also by lesions of the complex cartilage and ligamentous apparatus of the temporomandibular joint itself and, last but not least, by damage to the bone in the joint area. The clinical picture is also referred to as craniomandibular dysfunction (CMD).
Not every cracking when opening the mouth or chewing requires treatment. Approximately 70% of the population exhibit such symptoms without any evidence of illness. However, if there is pain when opening the mouth or dysfunction when chewing, a doctor should be consulted.
Temporomandibular joint complaints that require diagnostic clarification are
- Cracking or rubbing noises in the temporomandibular joints with pain when chewing or speaking.
- A painfully restricted mouth opening or closing and a deviation of the lower jaw to one side when opening the mouth.
- Swelling and redness of the soft tissue around the cheeks and temples.
- Pain in the temporomandibular joints with radiation to the ears, temples, neck, back of the head or shoulders.
After a detailed clinical assessment and a basic radiological diagnosis, a significant improvement in the findings is achieved in most cases through short-term physiotherapy. In some cases, however, further diagnostics (e.g. MRI) are necessary. Splint therapy is then often recommended. This involves a plastic splint that has to be specially adapted to the patient's requirements and is usually worn at night. The aim is to relax the masticatory muscles and relieve pressure on the temporomandibular joint.
If conservative measures have not been successful, adjuvant surgical therapy may also be necessary.
In maxillofacial surgery, minimally invasive procedures such as arthrocenthesis or arthroscopy are available in addition to open surgical measures, in which the temporomandibular joint is opened via access routes in front of or behind the ear. In the case of severe degenerative diseases with destruction of the bone in the articular process area, it may also be necessary to insert an artificial temporomandibular joint prosthesis.
If you have any complaints or would like advice on the subject, please make an appointment with the clinic office
Tel. +41 61 265 70 70
Fax. +41 61 265 70 71
Craniofacial malformation
Craniofacial malformations are rare and are caused by a variety of disorders of normal developmental processes and regulatory control mechanisms of growth. These disorders can be congenital (genetic) or acquired, they can occur in isolation or as part of complex syndromes and are usually accompanied by clearly visible malformations of the face or the entire head. In syndromic malformations, other organ systems are often also affected. The severity of craniofacial anomalies is highly variable and ranges from slight asymmetries and malpositioning of the jaws to conspicuous malformations of the face or the entire head with severe functional limitations of all organ systems involved. In addition to the aesthetic features, this can result in impaired brain growth, impaired vision, swallowing and speech disorders or involvement of the external ear and sense of hearing, severely impairing the development of those affected.
Examples of the most common craniofacial developmental disorders:
- Craniosynostoses (adhesions of the cranial sutures, to be distinguished from positional head deformities (see below)): The fusion of cranial sutures results in typical cranial deformities under the growth pressure of the brain, depending on the pattern of the affected sutures, which cannot correct themselves spontaneously. If brain development is impaired by the resulting constriction, developmental disorders can occur.
- Position-related head deformities: A lack of space in the uterus or incorrect positioning after birth can lead to deformities of the skull that are not caused by premature closure of the cranial sutures and do not require surgical correction. Such head deformities can be efficiently corrected in the first year of life through physiotherapeutic adjustments (including chiropractic/osteopathy) and/or the fitting of an individually designed helmet.
- Complexcraniofacial mal formations: The causes of complex craniofacial malformations are varied and in some cases still unknown. Disorders of growth control due to genetic mutations are assumed, for example, in the most common craniofacial syndromes (Apert syndrome, Crouzon syndrome, Pfeiffer syndrome, Saethre-Chotzen syndrome, etc.). These syndromes show a typical malformation pattern with a short, broad skull, receding midface and upper jaw, protruding eyes and an apparently enlarged lower jaw (malocclusion) in widely varying degrees. There is often a combination with adhesions of the cranial sutures (craniosynostosis), more rarely a cleft palate (e.g. Apert syndrome) or involvement of the skeletal extremities (e.g. Apert syndrome).
- In Treacher-Collins (Franchescetti) syndrome, a mutation in the gene sequence responsible for facial development leads to typical malformation features with underdevelopment/absence of the zygomatic bone, receding lower jaw, malformations of the ear and hearing impairment, malformations of the eye and eyelids. Cleft palates are often observed.
- Facial asymmetries are quite common and do not necessarily require surgical correction if they are minor. They can occur in connection with jaw malpositions or in the context of pronounced malformations (e.g. hemifacial microsomia (half-sided underdevelopment of one half of the face). In the case of esthetic functional impairment, skeletal corrective surgery, contour improvements and soft tissue augmentation (e.g. lipofilling) are indicated.
The treatment of craniofacial malformations is complex and is provided by interdisciplinary teams of specialists (maxillofacial surgery, neurosurgery, ENT, orthodontics, pediatrics, ophthalmology, logopedics and myofunctional therapy, physiotherapy and osteopathy, geneticists) at every stage of treatment. In the case of pronounced disorders, years or lifelong care is often necessary. Treatment at the USB is based on the latest scientific findings and is planned and carried out individually in close cooperation with specialists from other disciplines. The experienced medical team has access to the latest planning methods (3D analysis and simulation, 3D printing, navigation, etc.).
We will be happy to advise you in detail in our special consultation hours. Please make an appointment with our clinic secretariat
Tel. +41 61 265 70 70
Fax +41 61 265 70 71
Implantology and pre-prosthetic surgery
The restoration of chewing function using artificial tooth roots (dental implants) is an established standard procedure in modern oral and maxillofacial surgery. Implants made of pure titanium or titanium alloys are anchored directly in the jawbone. This allows either a fixed denture to be inserted or the fit of a removable denture (prosthesis) to be improved.
Nowadays, cylindrical or screw-shaped implants with different surface treatments are preferred. After a healing phase of 3-6 months - or sooner in some cases - the implants are fitted with crown/bridge constructions or telescopic or bars to secure a removable denture.
If the jaws have been edentulous for a long time, bone loss may occur. In such cases, a prosthetic restoration can be difficult, sometimes even impossible. There is also a risk of spontaneous mandibular fracture in cases of extreme bone loss. In such cases, bone material must be transplanted in preparation for implantation before a planned restoration with implants. Depending on the extent of the bone loss, artificial bone replacement materials or autologous bone from the regional area (e.g. lower jaw: chin, jaw angle) are used. If a larger amount of bone is required, it may also be necessary to remove bone from the pelvic blade.
These procedures can usually be performed under outpatient conditions. In some patients, general illnesses can make implantation more difficult, e.g. bleeding tendencies due to the use of anticoagulants (e.g. Marcoumar). In such cases, the clinical infrastructure at the University Hospital Basel allows us to adjust the blood coagulation before the operation - if necessary under inpatient conditions.
We coordinate the planning and implementation of an implant-supported dental prosthesis closely with your family dentist. If you are interested, you can make an appointment for a consultation with the clinic secretary during the consultation hours of the senior dentists, or arrange for your family dentist to refer you directly Tel. +41 61 265 70 70, Fax. +41 61 265 70 71.
Obstructive sleep apnea syndrome
Snoring or apnoea during sleep can indicate an obstruction of the upper airways as part of obstructive sleep apnoea syndrome (OSAS). Although there is also a central form of this respiratory arrest, which is based on a disturbance of the respiratory drive, this is much rarer (90:10).
The severity of OSA is diagnosed by means of monitoring in the sleep laboratory. The diagnosis and treatment of OSAS is carried out on an interdisciplinary basis by specialists in pulmonology and ENT and, if necessary, by other disciplines.
In obstructive sleep apnoea, the upper airways are mechanically obstructed by a flaccid tongue and the surrounding tissue, preventing oxygen-rich air from reaching the lungs in sufficient quantities. The lack of oxygen leads to wake-up reactions, which can trigger a number of secondary diseases, including high blood pressure, heart disease and stroke. Typically, this leads to performance-impairing daytime sleepiness (microsleep).
In addition to the soft tissue problems mentioned above, the cause of obstruction of the upper airways may also be found at the skeletal level. As the tongue musculature is partially attached directly to the lower jaw, a small receding lower jaw or an unfavorable position of the lower jaw during sleep can provoke an obstruction of the airways and thus promote OSA. In such situations, so-called positioning splints ("snoring splints"), which are worn during the night, similar to an orthodontic appliance, can be used therapeutically; in special cases, skeletal repositioning surgery (moving the jaws forward) may be necessary.
The therapeutic concept is developed individually for each patient after a detailed interdisciplinary analysis and includes a range of conservative measures (weight reduction, stopping smoking, reducing alcohol consumption, changing sleeping position, snoring splint, pressure mask, tongue stimulator, etc.) as well as soft tissue surgery on the tongue and soft palate or jaw repositioning surgery.
We are happy to answer any questions you may have or provide comprehensive advice.
Please contact us on the following telephone number
Phone +41 61 265 70 70
Fax +41 61 265 70 71
Plastic, reconstructive and aesthetic facial surgery
Plastic-reconstructive surgery of complex injuries and damage to the mouth, jaw, face, neck and skull region following tumor operations, serious accidents or the correction of congenital malformations is a branch of oral and maxillofacial surgery.
Precise knowledge of the anatomy and function of the facial region and the bony foundation (forehead, midface, jaw, nose) is the most important prerequisite for the optimal planning and execution of aesthetic facial procedures. The day-to-day handling of all surgical procedures in the facial area enables the oral and maxillofacial surgeon to safely perform individual therapies - from skeletal repositioning surgery, profiloplasty and rhinoplasty to pure soft tissue corrections such as facelifts, eyelid correction or wrinkle treatments.
For consultations, please make an appointment via the secretariat in Prof. Hans-Florian Zeilhofer's private consultation, tel. +41 61 265 73 44.
Skull base and orbital surgery
The bony base of the skull represents the boundary between the facial skull and the cranium. Injuries or tumors in this area are a challenge for surgeons, as there are particularly close relationships between highly vulnerable anatomical structures (nerves, blood vessels, etc.), the loss of function of which would severely impair the patient's quality of life or be incompatible with life. For this reason, affected patients are treated by a team of highly qualified specialists from various fields (oral and maxillofacial surgery, neurosurgery, otorhinolaryngology, etc.).
The most modern imaging procedures are available at the University Hospital for diagnostic purposes. New planning procedures for the three-dimensional representation of individual patient anatomy are used in surgical preparation. Systems for intraoperative navigation ensure that the surgical plans are transferred to the surgical environment. Patients also benefit from the clinic's excellent equipment during the operation: new procedures for processing hard tissue allow particularly gentle surgical techniques.
Patients can make an appointment via the clinic secretary's office during the consultation hours of the senior physicians or arrange a referral directly through their family doctor Tel. +41 61 265 70 70, Fax. +41 61 265 70 71. The presentation to the interdisciplinary treatment team will be organized by your attending senior physician.
Spheno-orbital meningioma: cure thanks to interdisciplinarity
Affiliated wards and outpatient clinic
