
Gynecology and gynecologic oncology
In gynaecology, we offer a wide range of diagnostic and therapeutic specialties and specialized treatments. All gynaecological surgical procedures are carried out by highly specialized teams using state-of-the-art technical equipment.
In addition to the general gynecological consultation hours, there are numerous special consultation hours run by certified specialists, e.g. for endometriosis, fibroids or changes in the vulva. If you have an abnormal cancer smear, ovarian cysts or if an ultrasound is indicated in gynecology, we will be happy to assist you with the knowledge of our experienced, constant team and state-of-the-art examination procedures.

Prof. Viola Heinzelmann-Schwarz
Co-Leiterin Frauenklinik
Chefärztin Gynäkologie/Gyn. Onkologie
The gynecological outpatient clinic of the Women's Clinic is located on Vogesenstrasse and is used for consultation and treatment of dysplasia, colposcopy and vulva consultations and manual ablative procedures.

The gynecological oncology department is located on the second floor of Spitalstrasse 21. An interdisciplinary team will work with you to develop a treatment plan tailored to your needs and clinical picture. Please feel free to contact us!

Gynecological diseases of women
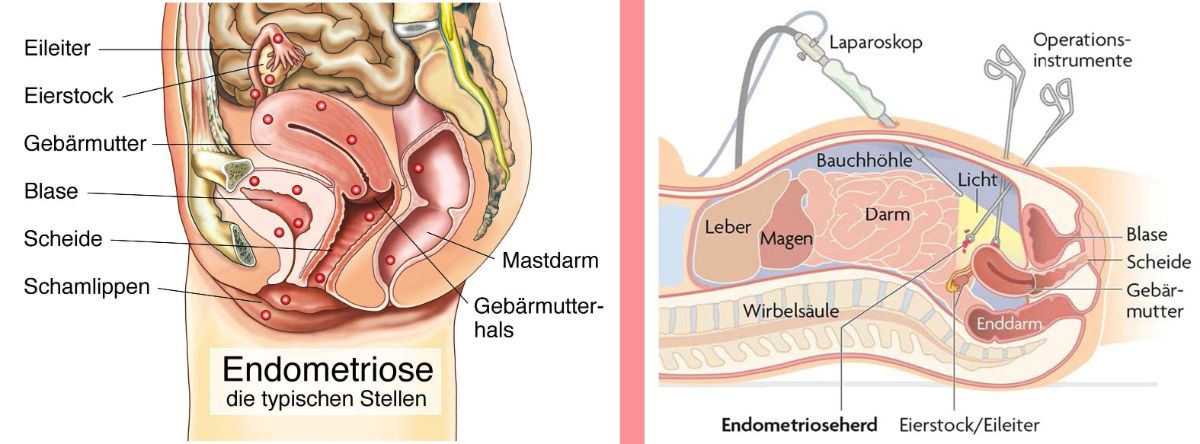
Endometriosis
Endometriosis is a benign disease in which the lining of the uterus settles outside the uterine cavity, for example on the peritoneum, ovaries, bladder or bowel. The exact cause of this is not known.
Endometriosis is one of the most common benign women's diseases. It impairs physical well-being, can have psychological consequences and can put a strain on a relationship. It is estimated that 10% of women of childbearing age and up to half of women who are unable to conceive are affected. Endometriosis manifests itself with a wide variety of symptoms.
Sometimes it is dominated by pain, in other cases it leads to involuntary childlessness or the impairment of organ systems. The variety of symptoms is one reason why endometriosis is sometimes only discovered years later.
Diagnosis
It is important to take a detailed history and record the symptoms. In addition to the various pains, it is also important to discuss any desire to have children and to assess the woman's individual life situation. This is followed by a gynecological examination, which is generally supplemented by a vaginal ultrasound. Depending on the situation, further examinations may be carried out.
Therapy
In addition to surgery, there are symptomatic (painkillers), hormonal and complementary therapies.
As the individual situation and symptoms of the woman are always different, there is no standard therapy. The therapy must be adapted to the woman, whereby a combination of surgical and hormonal therapy often brings the greatest success.
Laparoscopy
A laparoscopy is an important part of the treatment of endometriosis. During the endoscopy, the abdominal cavity must first be filled with gas (carbon dioxide). A camera is then used to look through the navel into the abdominal cavity. The camera provides magnification. The endometriosis lesions are removed using special instruments with a diameter of 3-5 mm. Compared to an abdominal incision, laparoscopy not only offers better cosmetic results, it also causes less pain and shortens the hospital stay.
Here you can learn more about the clinical picture of endometriosis and find out about the various treatment options available at our center:
What is the cause of endometriosis?
The causes of endometriosis are not yet fully understood. There are various theories, but none that can explain all phenomena and symptoms. Some possible causes and risk factors are
- Retrograde menstruation: it is assumed that menstrual blood, which normally flows out of the uterus via the vagina, flows back into the abdominal cavity through the fallopian tubes. This blood, which carries endometrial cells, can colonize and grow outside the uterus. It produces substances that ensure that blood vessels and nerves grow into the mucosal tissue (= endometriosis): these take over the supply of the newly formed endometriosis lesions.
- Endometriosis releases various substances that have an inflammatory effect and cause pain. They can also bleed during your period, which can lead to the development of adhesions as well as inflammation.
Why does endometriosis occur in some cases?
Normally, this uterine lining is broken down again by cells of our immune system (= the body's own defense system). However, various mechanisms can lead to this breakdown not working properly.
- Genetics: There are indications that endometriosis can occur more frequently in families, which suggests genetic factors.
- Immune system: Changes in the immune system may play a role in that they can promote the growth of endometrial cells outside the uterus.
- Hormonal influences: As the disease mainly occurs during the reproductive phase and endometriosis reacts to hormonal changes (pregnancy).
How is endometriosis diagnosed?
- Anamnesis (patient interview): a detailed anamnesis will be taken to establish the symptoms, medical history and possible risk factors.
- Physical examination: A gynecological speculum and palpation examination will be performed to detect any initial signs, such as enlarged or painful ovaries or to identify painful areas in the pelvis.
- Imaging procedures: Ultrasound is used to identify abnormalities. A transvaginal ultrasound examination can be particularly helpful. In some cases, an MRI (magnetic resonance imaging) can also be used.
- Laparoscopy: The definitive diagnosis of endometriosis is often made by laparoscopy. This is a minimally invasive procedure in which a thin instrument with a camera (laparoscope) is inserted through a small incision in the navel. This allows the doctor to view the internal organs directly and identify endometriosis lesions. Tissue samples (biopsies) can also be taken during the laparoscopy to confirm the diagnosis.
Symptoms of endometriosis can often be similar to those of other diseases and an accurate diagnosis sometimes requires several examinations by specialists.
What forms of endometriosis are there?
Endometriosis occurs in different forms, depending on the localization of the tissue focus. The most common forms of endometriosis are
Peritoneal endometriosis: Here, endometriosis lesions grow on the inner layer of the peritoneum. These lesions can spread to various organs in the pelvic area, including the uterus, fallopian tubes, bladder and bowel. Most experts agree that it is caused by retrograde menstruation.
Ovarian endometriosis: This is where endometriosis lesions form on the ovaries. These foci can form cysts, so-called endometriomas or "chocolate cysts".
Deep infiltrating endometriosis (DIE): In this case, the endometriosis lesions penetrate deep into the surrounding tissue (over 5mm). This can lead to pain and adhesions. Localizations can be
- between the bowel and uterus or vagina (= rectovaginal endometriosis)
- between the bladder and the front wall of the uterus (= bladder endometriosis)
- on the ligaments that run between the uterus and sacrum (= sacrouterine ligaments)
- in the ligaments that fix the uterus in the pelvis (maternal ligaments = parametria)
- in the pelvic wall, especially near the ureters
Adenomyosis: This is a special form of endometriosis in which the foci of endometriosis are found in the muscle wall of the uterus (adeno = gland, myosis = muscle). One theory is that small injuries in the uterine wall, caused by the increased contractility, allow endometrial cells to penetrate the uterine wall and thus form adenomyosis. Presumably, more oestrogen is produced in the uterus of those affected, which in turn causes increased contractions of the uterus. Adenomyosis can cause almost all of the symptoms described above. It also leads to very heavy, irregular and/or prolonged bleeding.
Extrapelvic endometriosis: Rarely, endometriosis can also occur outside the pelvic cavity, for example in the:
- Abdominal wall (especially after previous abdominal surgery such as a caesarean section)
- navel
- Lungs or other organs of the body: The endometriosis cells reach these areas because they can also spread via the lymphatic system. This can lead to metastases in these organs.
How can endometriosis be treated?
Endometriosis is a complex and usually chronic disease. Due to the different life situations and complaints of those affected, there is no standard therapy. Treatment depends on the following factors
- Severity of the symptoms
- Extent of the disease
- Family planning
- Patient's wishes
These are some common treatment options:
Pain therapy: A sufficient intake of painkillers is essential in endometriosis therapy. In order to avoid chronification, painkillers should be taken at the onset of pain and in sufficiently high doses. As endometriosis is a chronic inflammatory disease, it is important to use anti-inflammatory painkillers (non-steroidal anti-inflammatory drugs (NSAIDs)), e.g. products such as ibuprofen, diclofenac, naproxen or mefemanic acid. Preparations containing paracetamol are less suitable. For chronic pain in particular, it is advisable to contact our pain specialists.
Hormone therapy: As endometriosis is a hormone-dependent disease, treatment with hormones (especially pills containing progestogens) is advisable. This has a growth-inhibiting effect on the lining of the uterus and therefore also on the endometriosis lesions, as long as the progestogens are used. However, the hormones do not provide a cure: if you stop taking the pill if you want to have children or are intolerant, the endometriosis lesions can flare up again. The symptoms can also be improved with a combined contraceptive pill (pill with oestrogen and progestogen). It is best to take the pill without a break (long cycle) to reduce the amount of menstrual bleeding. Inserting a hormone coil into the uterus has also proven to be effective. In the case of pronounced findings, it sometimes makes sense to stop all oestrogen production in the body and to put the patient into a so-called artificial menopause. The withdrawal of oestrogen causes the foci to dry out. All these hormonal therapies often result in the absence or at least reduction of menstrual bleeding. This is an important goal of therapy, as it can prevent the further spread (or recurrence after surgery) of endometriosis.
In some cases, however, hormonal therapy is not possible or advisable - e.g:
- in the case of extensive findings that do not respond adequately to hormonal therapy
- in patients who complain of severe side effects from hormonal therapy that they cannot tolerate
- if they wish to have children, as the hormones prevent ovulation from taking place.
Surgical therapy: The aim of this surgical therapy is to remove all endometriosis lesions. In most cases, the operations are performed by laparoscopy. If neighboring organs are affected, more extensive operations are sometimes necessary. Another aim is to prevent or remove secondary symptoms such as scarring or adhesions. The function of the fallopian tubes can also be tested if there is a simultaneous desire to have children. In severe cases or if there is no longer a desire to have children, a hysterectomy (removal of the uterus) may be considered. After the operation, the tissue is examined to definitively confirm the diagnosis.
Treatment of the unfulfilled desire to have children: Reproductive medicine techniques such as in vitro fertilization (IVF) can be considered here to increase the chances of a successful pregnancy. We work closely with the Department of Reproductive Medicine and Gynecological Endocrinology at the Women's Clinic.
Complementary therapy approaches: Symptoms can also be alleviated by alternative therapeutic approaches such as acupuncture, physiotherapy, yoga, TCM (Traditional Chinese Medicine) or dietary changes.
We also offer supportive psychological care due to the psychological stress often caused by the disease.
Can endometriosis be cured?
So far, it can be said that there is no cure for endometriosis. However, targeted treatment can control the symptoms, improve quality of life and prevent secondary damage.
The choice of the best treatment option will be discussed with you individually.
Further information
Swiss Endometriosis Association: www.endo-help.ch/
Endometriosis Research Foundation: www.endometriose-sef.de
European Endometriosis League (EEL): www.endometriose-liga.eu
We work closely with interdisciplinary departments at the University Hospital, such as Surgery, Reproductive Medicine, Urology and Psychology, as well as with your gynecologist.
Management

Certification
Gynecological social medicine and psychosomatics
(incl. unwanted pregnancy)
Gynecological social medicine and psychosomatics
We often address topics that others don't or rarely ask about: disappointment, grief, anger. Addressing sensitive topics such as sexuality or violence professionally requires specialist expertise. We are trained in these issues and can offer you further points of contact. We see it as our job to be there in problem situations. We have noticed that women still do not know enough about their interests and needs and do not express them enough. We can help you to become more self-aware and more attentive to yourself. We support you in this. We take a holistic approach and pay close attention to what you bring to the table. There is no single form of therapy that we apply to you. We always adapt our therapies to each individual patient. In general, however, we pursue a solution-oriented approach.
Management

Unintended pregnancy
An unwanted pregnancy can trigger many feelings and questions. We are the pregnancy advice center of the Canton of Basel-Stadt and are open to all women seeking advice and their caregivers.
Counseling
Are you in a conflict situation? Do you have questions and need information for your decision? Would you like a neutral discussion about your personal situation?
What we offer
At our advice center you can discuss your situation in peace and you will receive all the information you need to make a self-determined decision. If you wish, we can refer you to other internal and external services. If you decide to terminate your pregnancy, we will initiate the necessary steps for a medical or surgical abortion. As a rule, a vaginal ultrasound examination is carried out before the abortion.
We are also there for you after the abortion. If you have any questions about contraceptive methods or other sexual health issues, you can also contact us.
If you wish, you can also come to the consultation with your partner or significant other.
Abortion
Termination of pregnancy can be performed using medication (up to nine weeks of pregnancy) or surgically (suction method). At your first appointment, after a gynecological examination with ultrasound, you will be informed about the procedure of the method you have chosen. The medical abortion is usually started on one of the following days and a follow-up check takes place two weeks later.
Legal basis
Abortions in Switzerland are regulated by the time limit solution (Art. 119 + 120 of the Swiss Criminal Code). During the first 12 weeks of pregnancy, you as a woman can decide whether you want to carry the pregnancy to term, terminate it or give the child up for adoption after birth. For an abortion after the 12th week of pregnancy, there must be a medically justified reason.
Costs
The costs of an abortion are covered by health insurance (less deductible and excess).
Further information
- Information on the subject of abortion from the BS Medical Services: https: //www.gesundheit.bs.ch/gesundheitsfoerderung/gesundheitsinformationen/schwangerschaftsa bbruch.html
- Sexual Health Switzerland: https://www.sexuelle-gesundheit.ch/
Myomas
Myomas are muscular nodules that can grow underneath the lining of the uterus, in the muscle wall or under the surface of the uterus. They can cause symptoms such as bleeding disorders, anaemia and pressure problems. In rare cases, fibroids can also cause premature pregnancy loss or pregnancy failure.
Management
There are three types of treatment for fibroids:
- Hormonal treatment
- Embolization of the blood vessels, i.e. interruption of the blood supply to individual fibroids
- Surgical therapy, which can range from the removal of individual fibroid nodes in women who wish to have children to the removal of the entire uterus
If you suspect endometriosis or fibroids, it is best to be referred to us by your gynecologist. Our team of experts will then advise you and your doctor individually.
Contact us
Women's Clinic
Spitalstrasse 21
4031 Basel
Monday to Friday
8.00-11.00 and 13.00-16.00
Ultrasound
A gynecological ultrasound examination is a diagnostic procedure for assessing the organs in the small pelvis (bladder, ovaries, fallopian tubes and uterus). High-frequency sound waves are used to create images of the internal genital organs.
These ultrasound images help to assess the following points:
- Clarification of complaints or unclear examination results
- Assessment of pathologically altered findings
- Support in therapy planning
- Control during the execution of a procedure (e.g. during a biopsy)
With the help of ultrasound examinations, diseases requiring treatment can be detected at an early stage. In addition, unnecessary check-ups, therapies or interventions can be avoided.
Ultrasound is used to assess the following complaints in women:
- Clarification of lower abdominal pain, genital bleeding, inflammation and genital abnormalities
- Assessment of the lining of the uterus (endometrium)
- Clarification of the pelvic organs in the case of an unfulfilled desire to have children
- Follow-up of findings in the small pelvis
- Diagnosis of tumors in the small pelvis
- Checking the position of IUDs
- Examination of the urinary bladder and determination of residual urine volume
Management

Prof. Gwendolin Manegold-Brauer
Stv. Chefärztin Geburtshilfe und Pränatalmedizin
Leitende Ärztin gynäkologische Sonographie und Pränataldiagnostik
FMH Gynäkologie und Geburtshilfe, FMH Schwerpunkt feto-maternale Medizin, DEGUM III für Gynäkologische Sonographie und pränatale Diagnostik

Urogynecology
Uro-gynecological conditions include bladder weakness (incontinence) and prolapse problems. The close proximity of the bladder, vagina, uterus and bowel often causes combined disorders. These conditions increase with age or after pregnancy and should be clarified in a specialized consultation.
Treatment options are
- Pelvic floor training
- bio-feedback
- physiotherapy
- Medication
- Pessary therapies
- operations
Management

Incontinence (involuntary loss of urine) can occur in two forms:
- Urge incontinence: Frequent urination, for example at night or when washing your hands.
- Stress incontinence: loss of urine due to a weakness in the bladder closure mechanism when coughing, running or laughing.
Both forms of incontinence can be caused by inflammation or other organ-related causes, which can often be treated quickly and easily once detected.
Prolapse of the female genital organs is often described as a foreign body sensation in the vagina or as a palpable finding at the entrance to the vagina and can lead to a considerable reduction in quality of life.
Furthermore, young women are examined for injuries to the pelvic floor after giving birth in our consultation hours. This mainly involves suture pain, birth injuries and tears in the rectal sphincter muscles during childbirth.
Sexual medicine
A fulfilling and satisfying sexuality makes a decisive contribution to human health. Sexual health is influenced by various factors - and our treatment approaches are correspondingly diverse.
Our focus is not just on eliminating a functional disorder. We deal with all aspects that influence your physical, emotional, mental and social well-being in connection with sexuality. This is why we work on an interdisciplinary basis with various medical disciplines, psychology and physiotherapy.
Management
Among other things, we are available to help individuals and couples with the following concerns:
- Questions about sexuality
- Lack of sexual desire (libido disorder)
- Arousal disorders
- Orgasm difficulties
- Pain during sexual intercourse (dyspareunia)
- Sexual difficulties with chronic illnesses (e.g. neurological or psychological)
- Sexual difficulties during or after cancer treatment
- Treatment offer for problematic sexual tendencies
Do you need an appointment or do you have any questions? Please feel free to contact us.
Monday to Friday
8.00-17.00
Tel: +41 61 265 93 93
Annual check-up for privately insured persons
At the Privatpraxis am Schützenhaus, we offer you state-of-the-art examination facilities for all gynecological issues in a dignified atmosphere. In the event that treatment is indicated for you, we naturally have access to expert diagnostics and the entire network of specialists at the University Hospital in order to achieve a rapid and holistic solution to your problem.
Gender matching
As part of the interdisciplinary innovation focus on gender variance, the University Hospital's gynecology department offers a consultation on the topic of gender reassignment. We will be happy to advise you and answer your questions in the practice at the Schützenhaus.
The consultation takes place on Friday afternoons.
Management

Ovarian cysts
Cysts are fluid-filled cavities in the ovaries and can develop due to various causes. Cycle disorders, inflammation, endometriosis or even tumors (benign and malignant) may be the cause. A gynecological examination including a transvaginal ultrasound is recommended to clarify cysts. If a cyst is larger than 5 cm, there is a risk of a so-called stalk torsion. This impairs the blood supply to the ovary, which can lead to severe pain.
Both hormone regulation and laparoscopy with cyst excision can be considered as treatment. This depends on the extent of the cysts and will be discussed with you individually.
It is best to be referred to our consultation by a registered gynecologist. We will examine you sensitively and advise you individually.
Management

Dr. André Kind MPH
Stv. Chefarzt Gynäkologie
Leitender Arzt GAF und Gynäkologische Dysplasieeinheit
Would you like some advice? Then please contact us using the following contact details:
Monday to Friday
8.00-17.00
Tel: +41 61 265 93 93
Your inpatient stay with us
Are you planning an inpatient stay? Our gynecological patients are on the Women's Clinic 4.2 ward. The individual needs and concerns of our patients and their relatives are central to our care. Our team looks after you around the clock and is always available to answer your questions.
Relevant information for your stay with us can be found here. Do you have any further questions? Please feel free to contact us at any time.
Visiting hours
The general visiting hours are from Monday to Sunday from 11.00 am to 8.00 pm. Individual arrangements can be discussed with our ward staff.
You are also welcome to visit our Giardino visitors' restaurant during opening hours.
Your entry
Before your inpatient stay with us, you will receive all relevant documents from our team. Do you have any questions? Please feel free to contact us!
Our premises
The Women's Clinic 4.2 offers all patients (with general and semi-private insurance) comfortable double rooms. Would you like a single room instead? Please contact us before your planned admission. We will be happy to discuss the rates and terms of payment with you. Please note that single rooms are limited and we cannot guarantee them.
You are also welcome to spend time in our cafeteria or the hospital garden. If you are scheduled to have examinations at this time, please cancel your stay at the ward office.
Investigations
If you are scheduled for examinations during your stay, please be ready on the ward. If you wish to leave the ward despite the scheduled examinations, please inform the ward office.
Where you can find us
Our ward is located on the 4th floor of Building B (formerly Clinic 1) at Spitalstrasse 21, 4031 Basel.
You can find directions to the University Hospital Basel here.
Management


Do you have direct questions for our station? Please feel free to contact us:
Phone: +41 61 265 92 31
Email: gyn.frauenklinik@usb.ch
